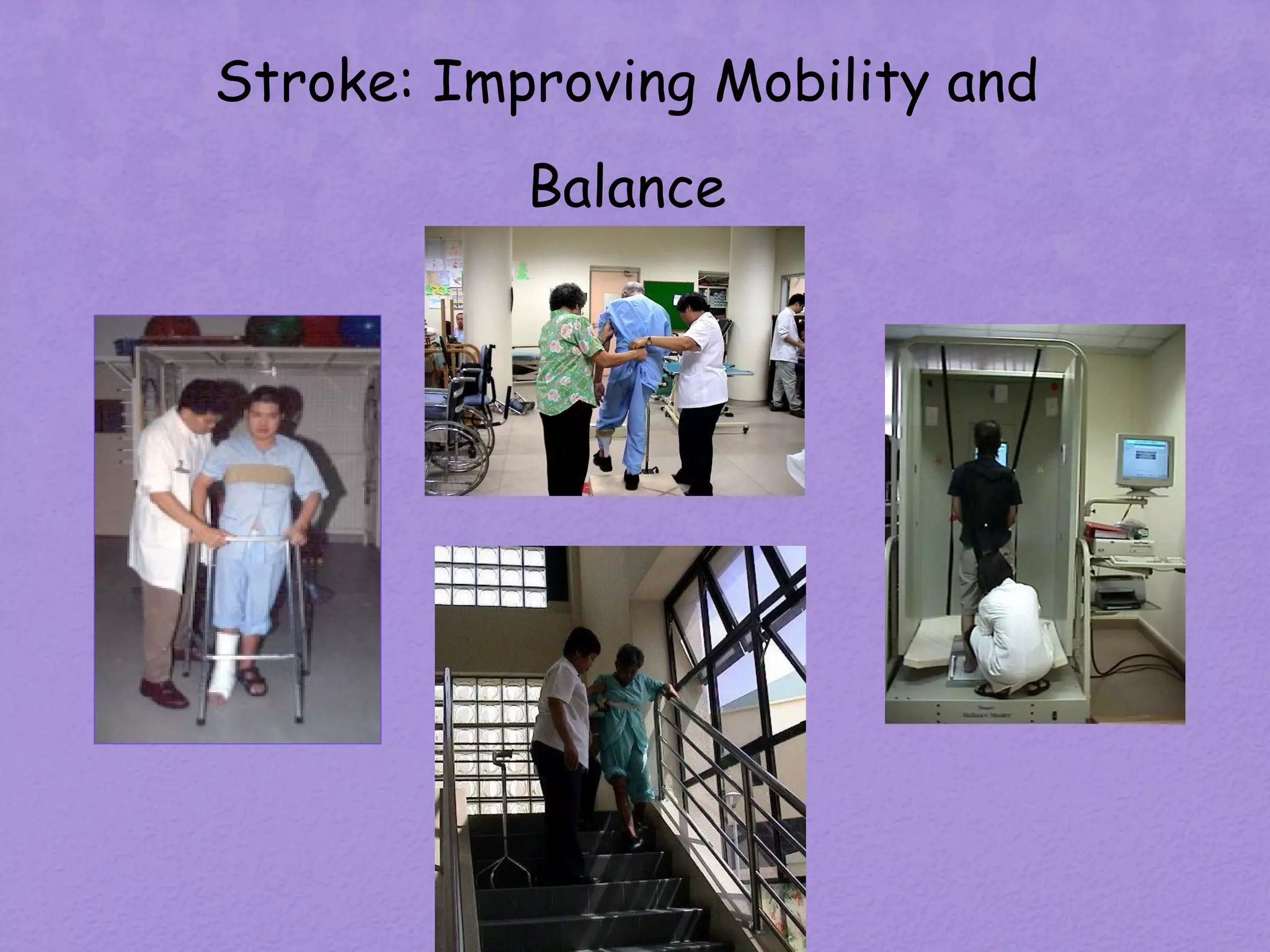
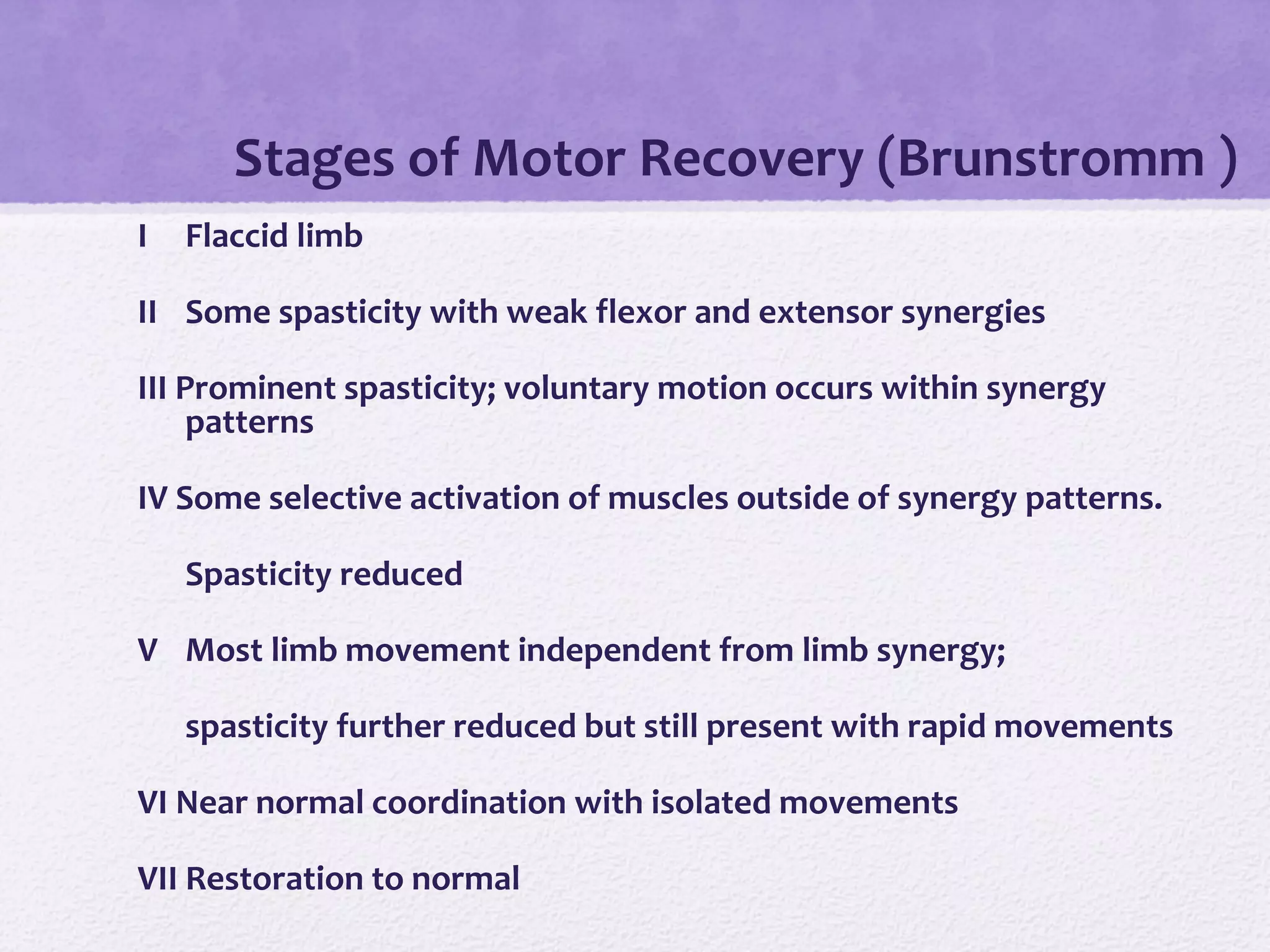
Stroke rehabilitation aims to help stroke survivors achieve their highest level of function and independence. It involves both neurological and functional recovery processes. The majority of neurological recovery occurs within the first 3 months post-stroke, while functional recovery may continue for longer with rehabilitation therapies. An interdisciplinary team provides comprehensive rehabilitation addressing impairments in areas like mobility, self-care, communication and cognition. Early mobilization and prevention of complications are important. Outcome measures assess different domains of recovery. Rehabilitation goals must be specific, measurable, achievable and timely.