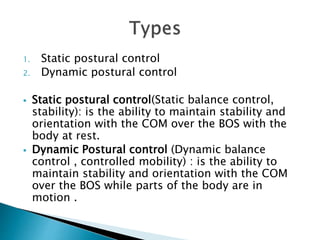
The document discusses postural control and balance, defining it as the ability to control body position in space. It describes static and dynamic postural control, and notes an intervention program should be based on an accurate evaluation. The summary provides exercises to improve postural alignment, control of movement, adaptation to tasks/environments, and fall prevention. A balance training program incorporates steady state, anticipatory and reactive exercises focusing on static and dynamic postural control.