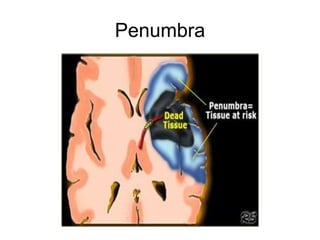
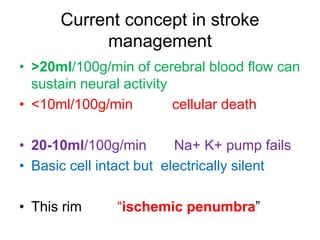
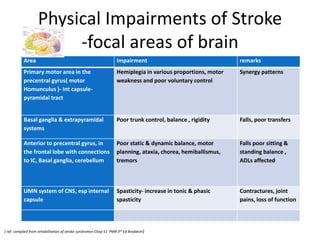
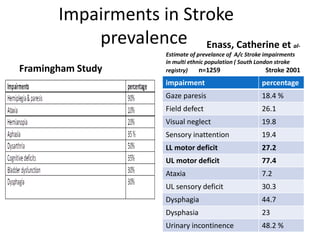
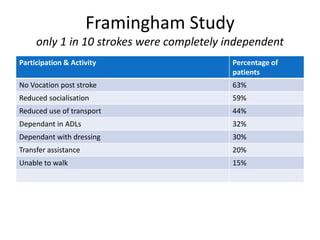
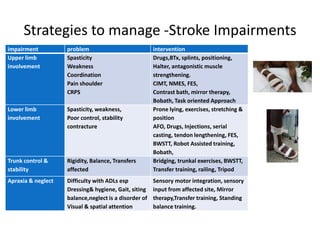
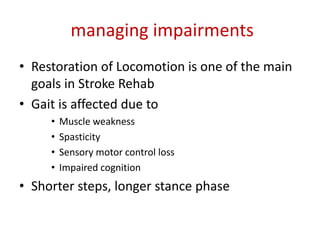
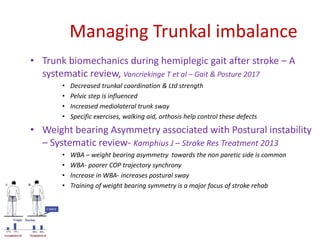
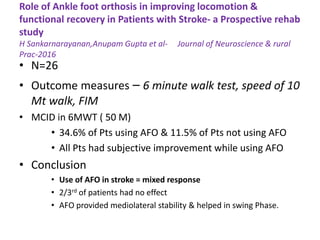
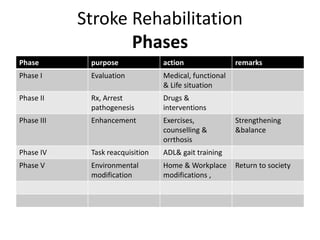
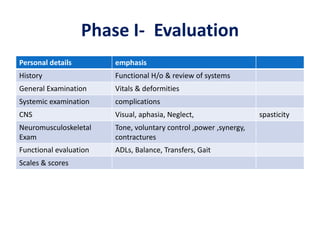
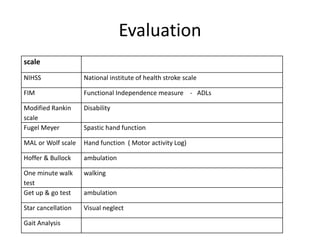
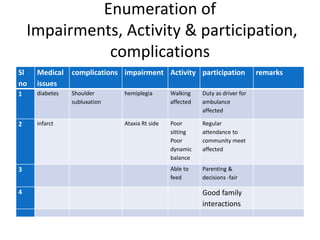
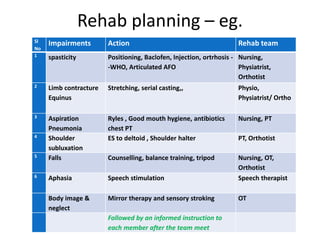
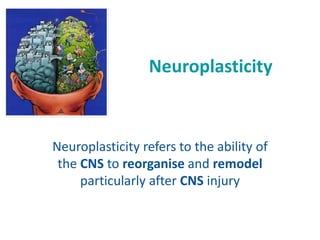
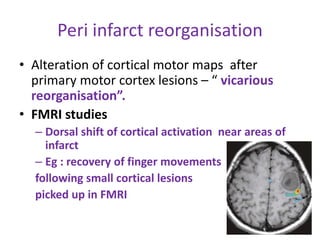
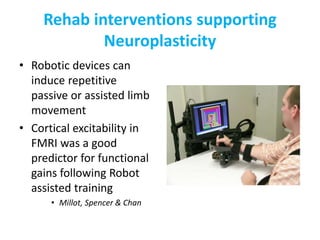
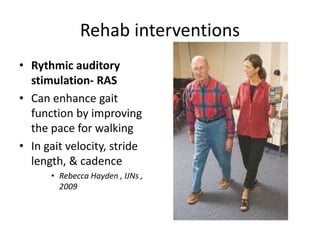
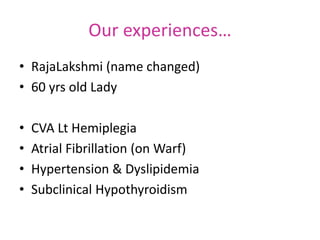
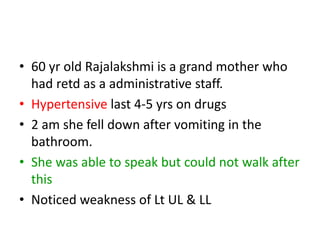
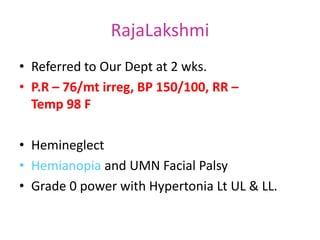
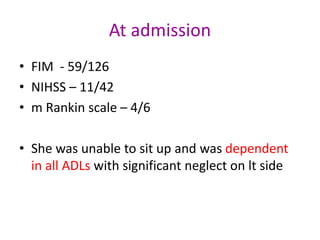
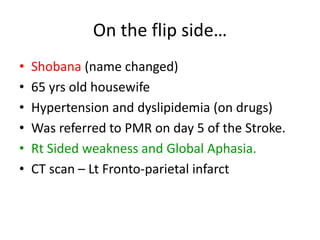
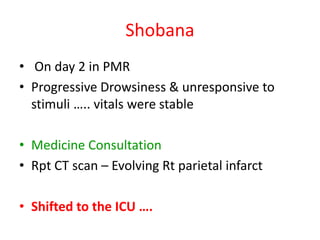
This document provides an overview of stroke rehabilitation and managing physical impairments. It defines stroke and discusses the importance of the ischemic penumbra in early rehabilitation. The document outlines the phases of rehabilitation and various interventions to address common impairments like weakness, spasticity, and balance issues. Evaluation tools and a sample rehabilitation plan addressing specific impairments are also presented.