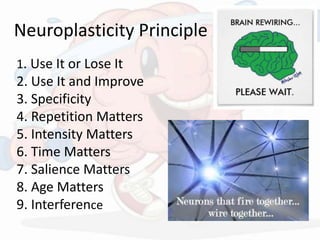
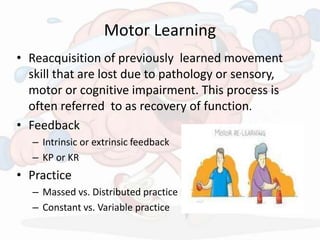
The document outlines practical guidelines for stroke rehabilitation, emphasizing the importance of a specialized neurorehab team and evidence-based approaches to recovery. It covers various aspects of management including acute care, ward management, and outpatient follow-up, along with strategies for enhancing functional recovery through techniques like early mobilization and tailored therapies. Key principles such as neuroplasticity and motor learning are highlighted as crucial for regaining skills and improving overall patient outcomes.



![Current Treatment Methods
• CIMT [Level 1]
• Bimanual Training[ Level 2]
• Mirror Therapy [LEVEL 2]
• Mental Imagery [Level 3]
• NMES/ FES [Level 2]
• EMG- Biofeedback [Level 3]
• Virtual Reality [Level 2]
• BWSTT [Level 2]](https://image.slidesharecdn.com/strokerehabppt2-160324124823/85/Practical-Guidelines-in-Stroke-Rehabilitation-15-320.jpg)
![Improving Trunk Control
• Trunk forms a foundation for any posture &
movement.
• Post hemi - loss of selective muscle activity in
trunk & tone - Compensatory movement is seen
• Rx focus on
-Trunk rotation, side flexion [all cardinal plane]
-Combination of movement
-Balance reaction[Anticipatory & Reactive]
-Functional Activity](https://image.slidesharecdn.com/strokerehabppt2-160324124823/85/Practical-Guidelines-in-Stroke-Rehabilitation-19-320.jpg)
![Improve UE Function
• Relearning of movt pattern & retraining of missing
component
• Upper body initiated wt shift pattern[reaching &
picking object]
• UL weight bearing & Dynamic stabilization exercise
• Functional movement & Combination movt
• Power production - Throwing
• Fine motor function- Object Manipulation
• Spastic Hand Rehab- Botox
• Adjuncts – Orthoses, CIMT, BF, NMES, VR, Robotics](https://image.slidesharecdn.com/strokerehabppt2-160324124823/85/Practical-Guidelines-in-Stroke-Rehabilitation-21-320.jpg)
![Improve LE function
• Strengthening muscles in appropriate pattern
& Functional pattern.
• Training for posterior weight shift, Anterior
weight shift & Lateral weight shift (sitting).
• Co-ordinated combination movement
• Power production [Kicking]
• Cycling & treadmill training](https://image.slidesharecdn.com/strokerehabppt2-160324124823/85/Practical-Guidelines-in-Stroke-Rehabilitation-22-320.jpg)