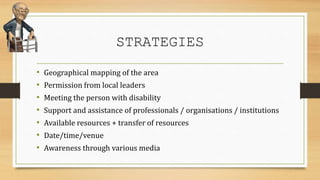
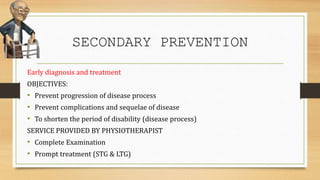
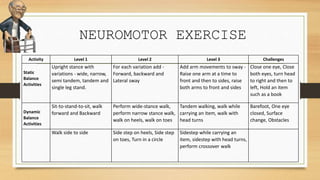
This document discusses geriatric management at both the individual and community level. At the individual level, management includes acute care, functional restoration, and prevention. Acute care focuses on education, pain relief, and healing. Functional restoration maintains and improves range of motion, strength, flexibility, and balance. Prevention maintains previous exercises and identifies risk factors. At the community level, a multidisciplinary team provides primary, secondary, and tertiary prevention. This includes health promotion, early diagnosis and treatment, and rehabilitation. The document also outlines exercise recommendations for older adults, including aerobic, strength, flexibility, endurance, and neuromotor exercises.