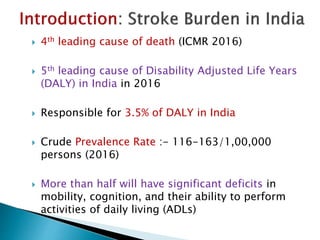
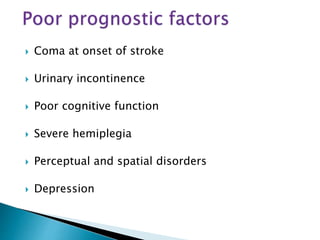
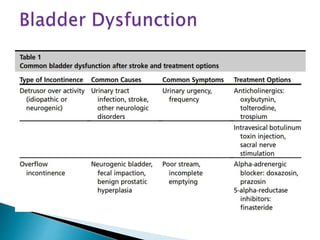
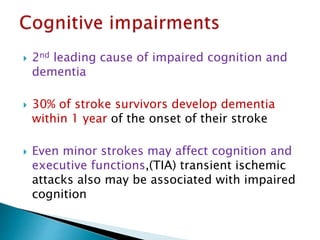
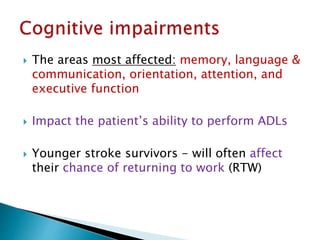
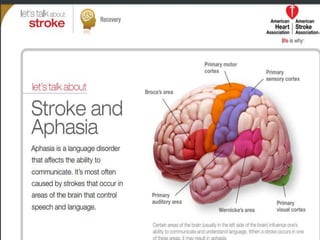
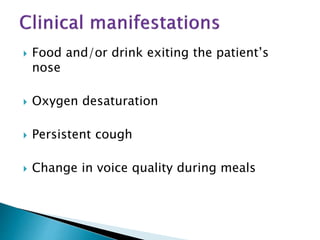
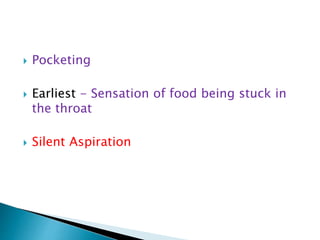
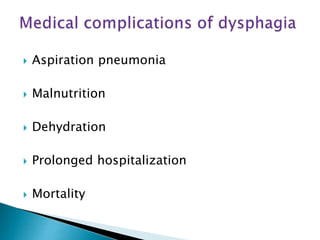
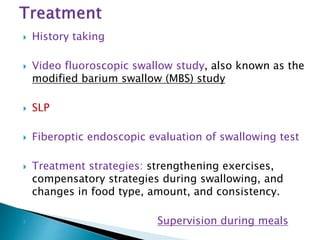
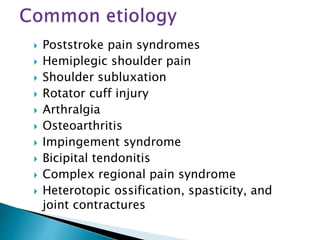
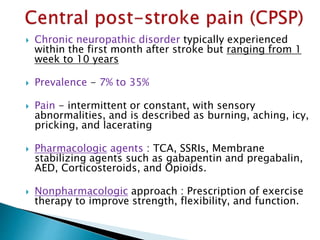
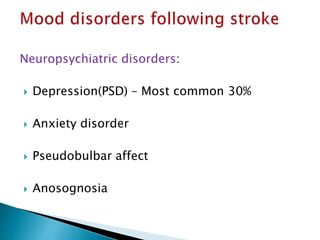
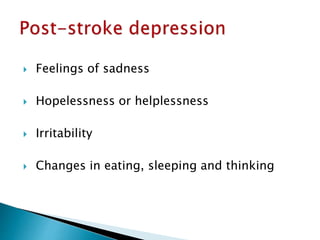
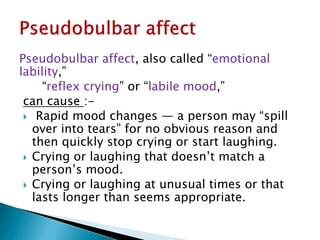
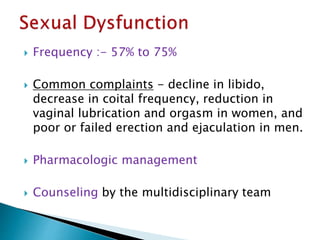
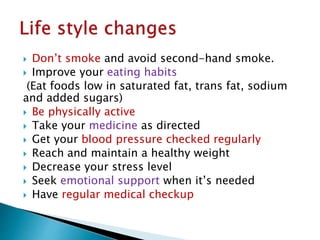
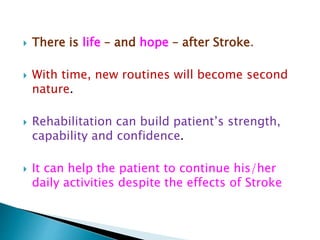
Stroke is a major cause of death and disability in India. Rehabilitation after a stroke aims to help patients regain independence and function through a team-based approach. Rehabilitation occurs in phases, beginning in the acute post-stroke period and continuing through outpatient care. It focuses on improving impairments, preventing complications, and enhancing quality of life through restoration and compensation strategies that capitalize on the brain's neuroplasticity. Common post-stroke impairments include motor deficits, cognitive issues, swallowing difficulties, and pain. An individualized rehabilitation plan incorporating exercise, therapy, and lifestyle changes can help patients achieve their goals.