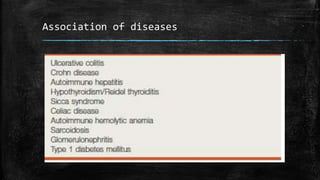
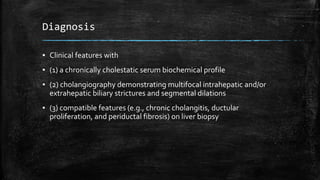
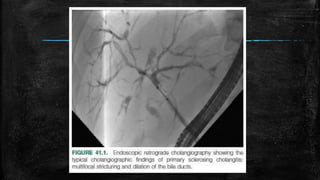
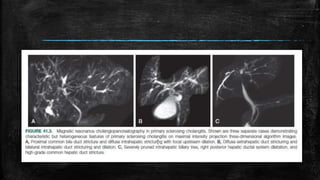
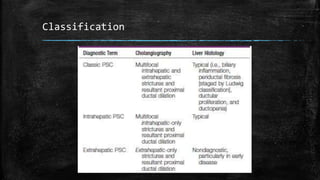
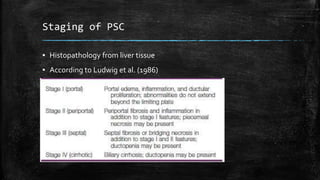
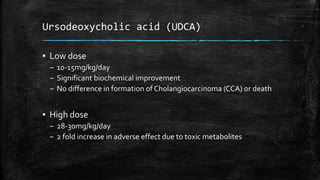
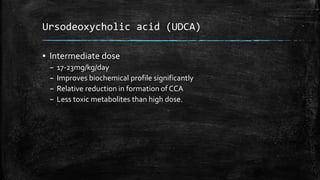
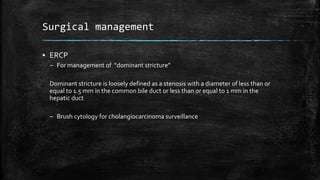
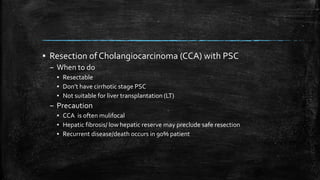
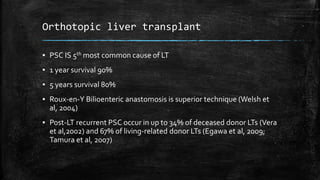
Primary sclerosing cholangitis (PSC) is a chronic liver disease characterized by inflammation and fibrosis of the bile ducts that can progress to cirrhosis and liver cancer. It has a median survival time of 15 years and is the fifth most common reason for liver transplantation. PSC commonly affects males in their 40s and is associated with inflammatory bowel disease. Diagnosis involves clinical features, blood tests showing cholestasis, and imaging or biopsy of the bile ducts. Treatment includes medications like ursodeoxycholic acid and antibiotics, as well as endoscopic procedures and ultimately liver transplantation for advanced disease.