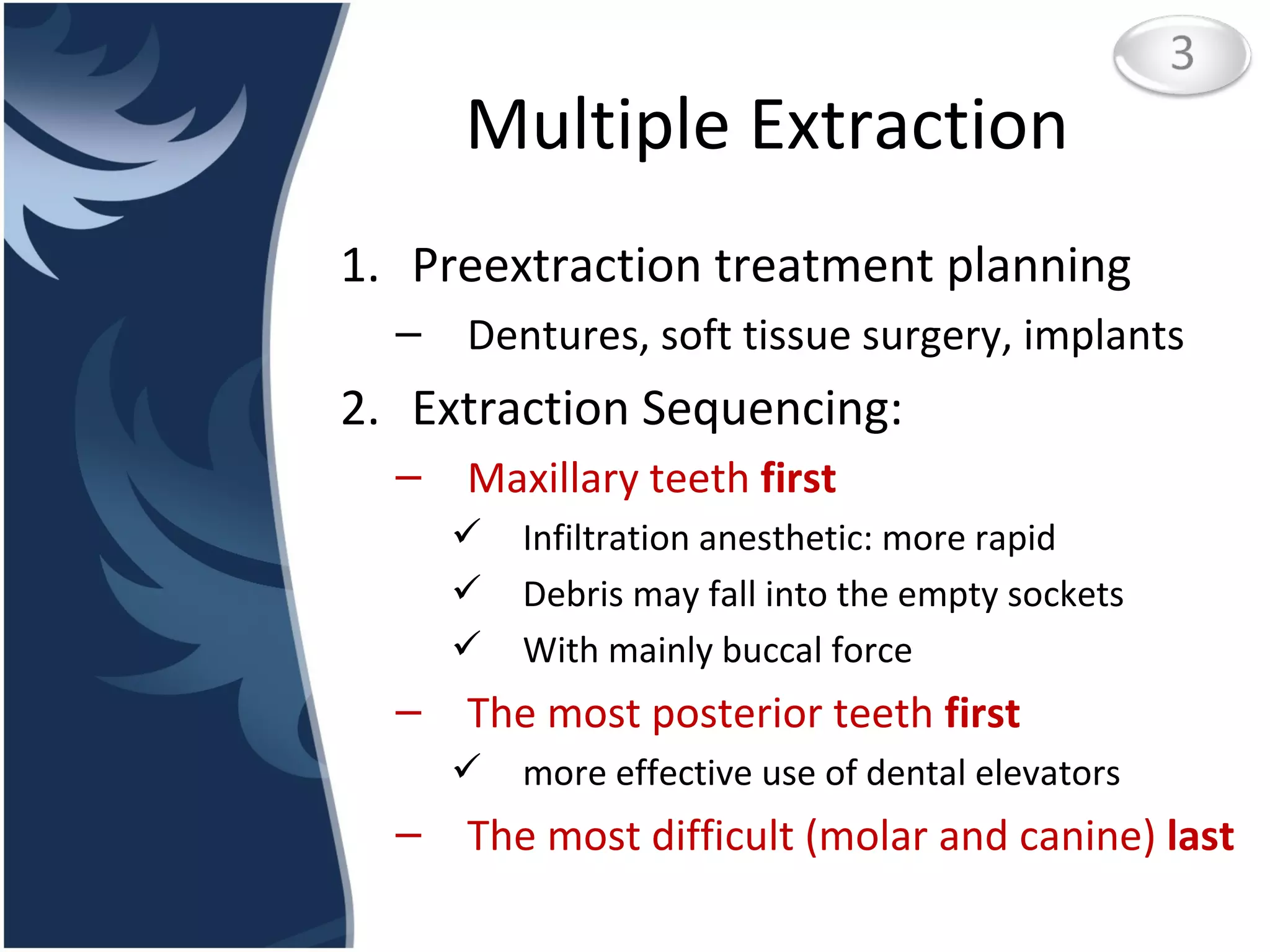
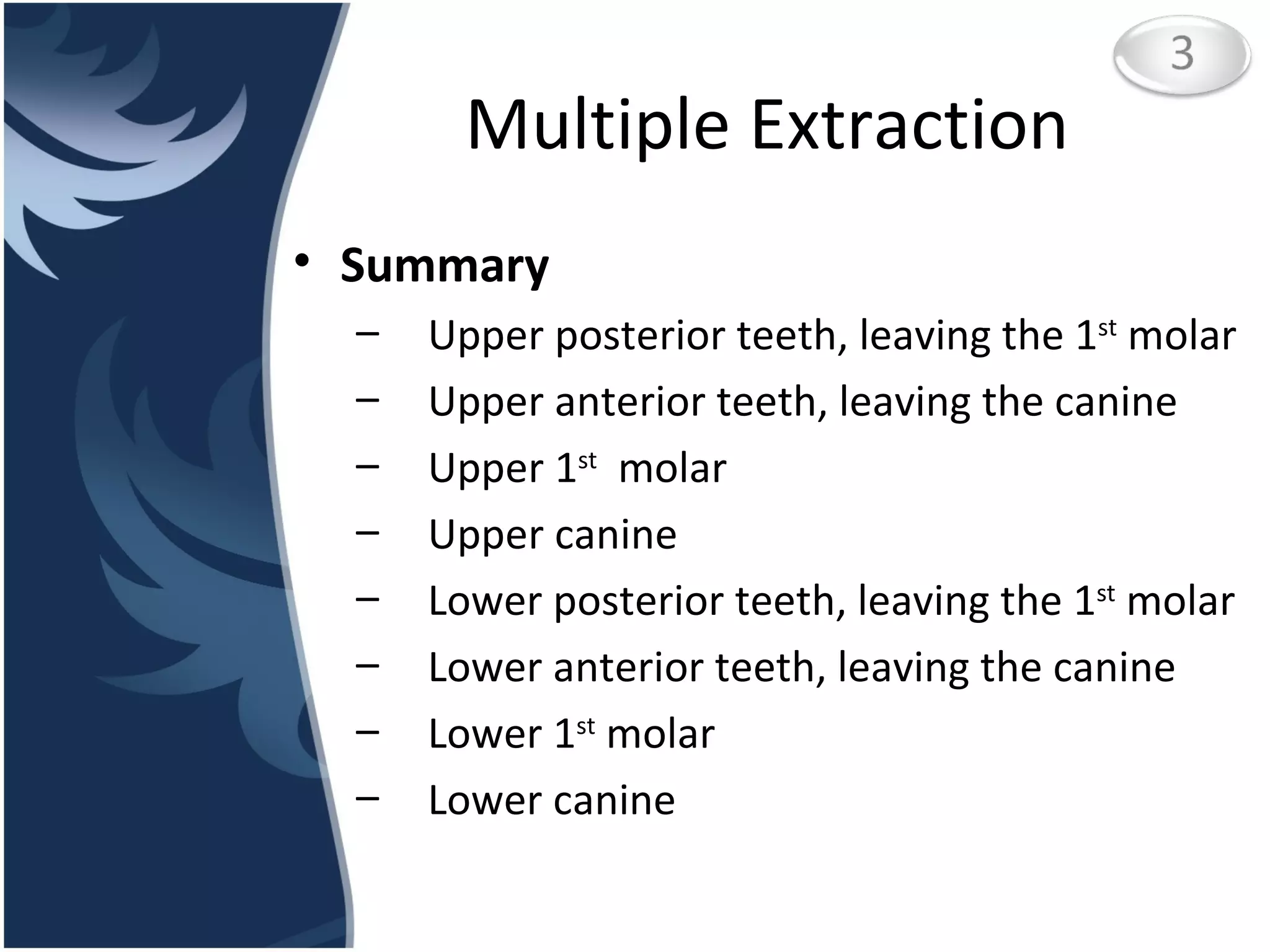
1. The document discusses surgical extraction of impacted and complicated teeth, including indications for surgery, classification of impacted teeth, surgical procedures, postoperative management, and potential complications.
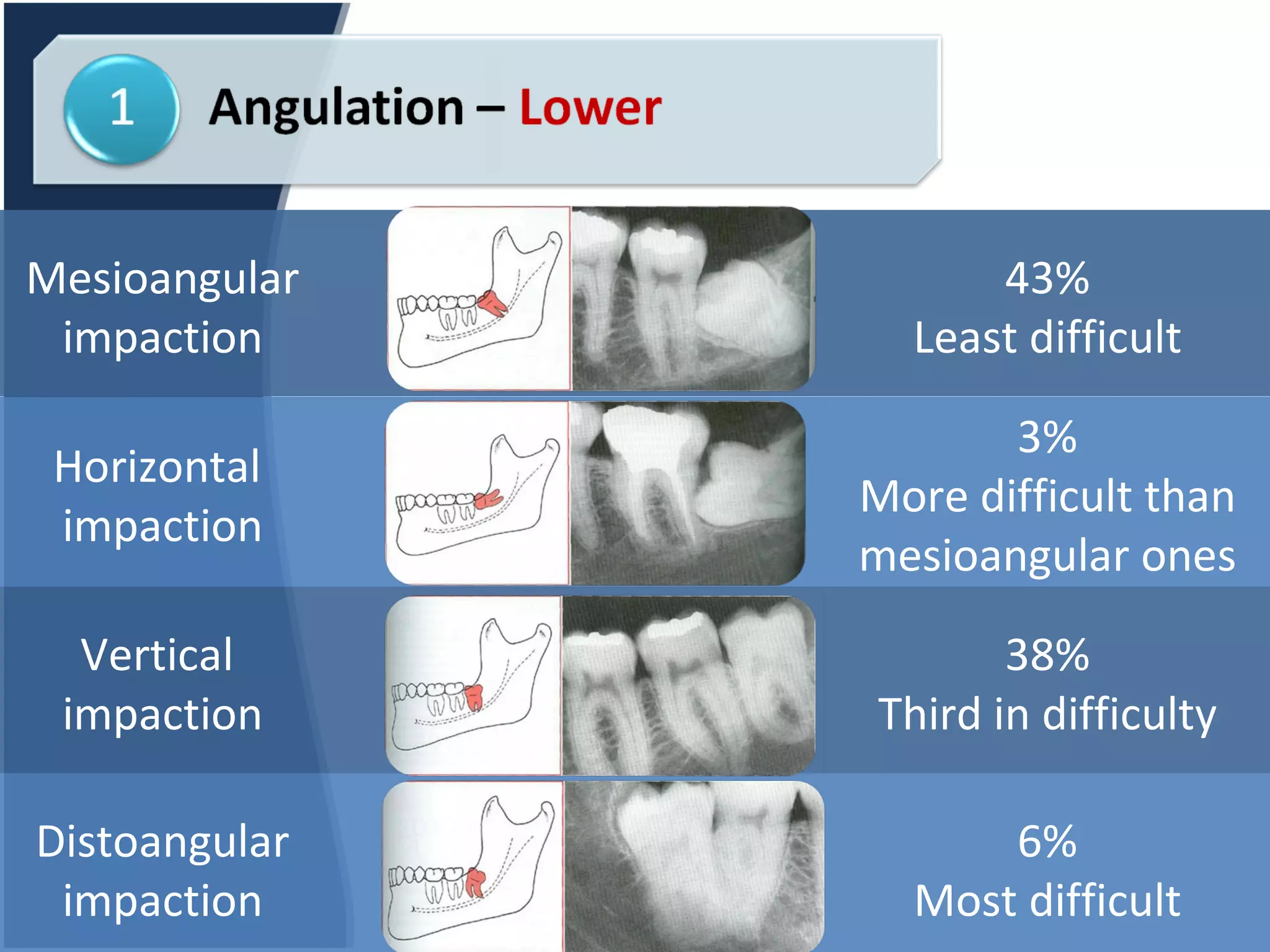
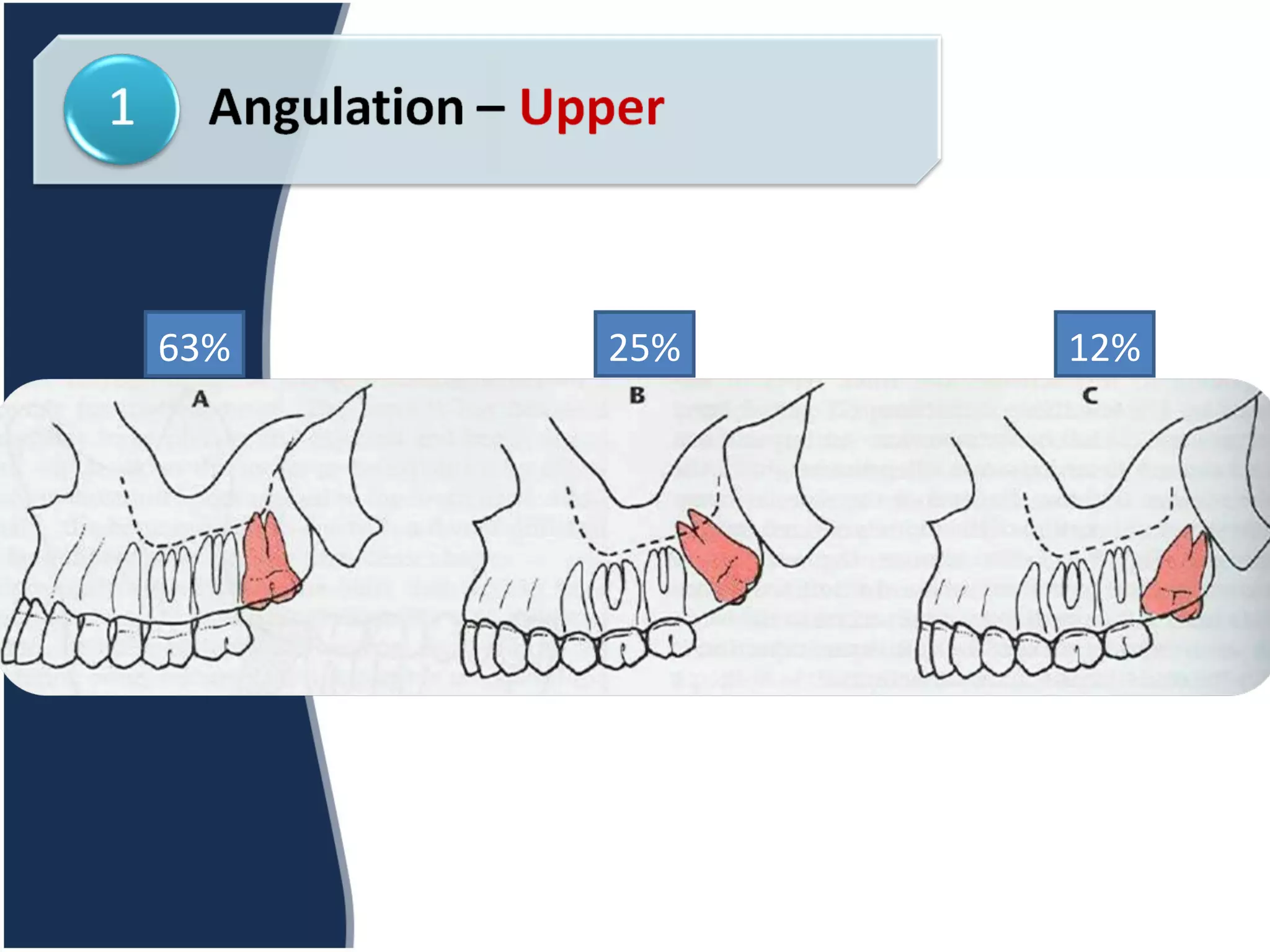
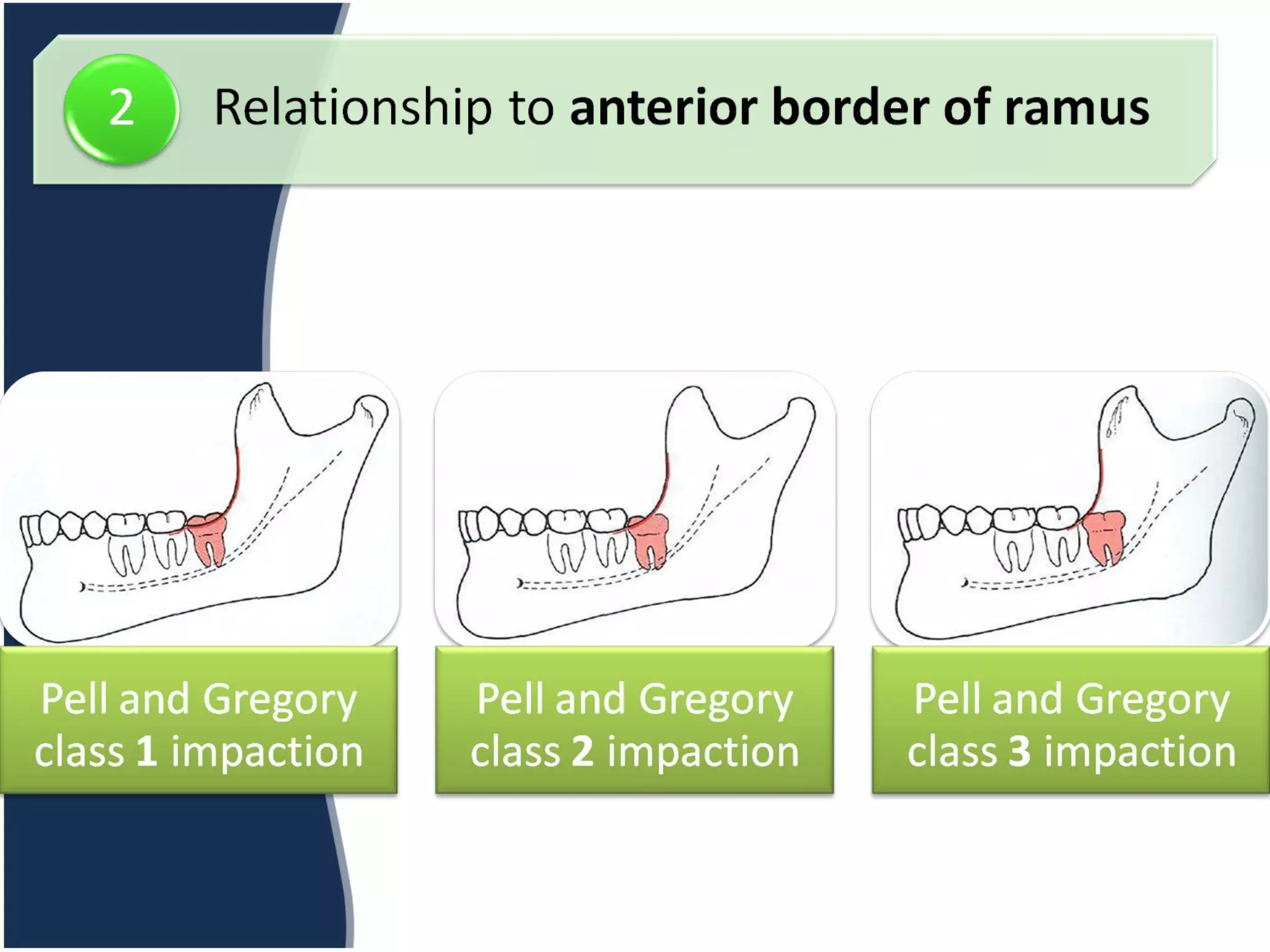
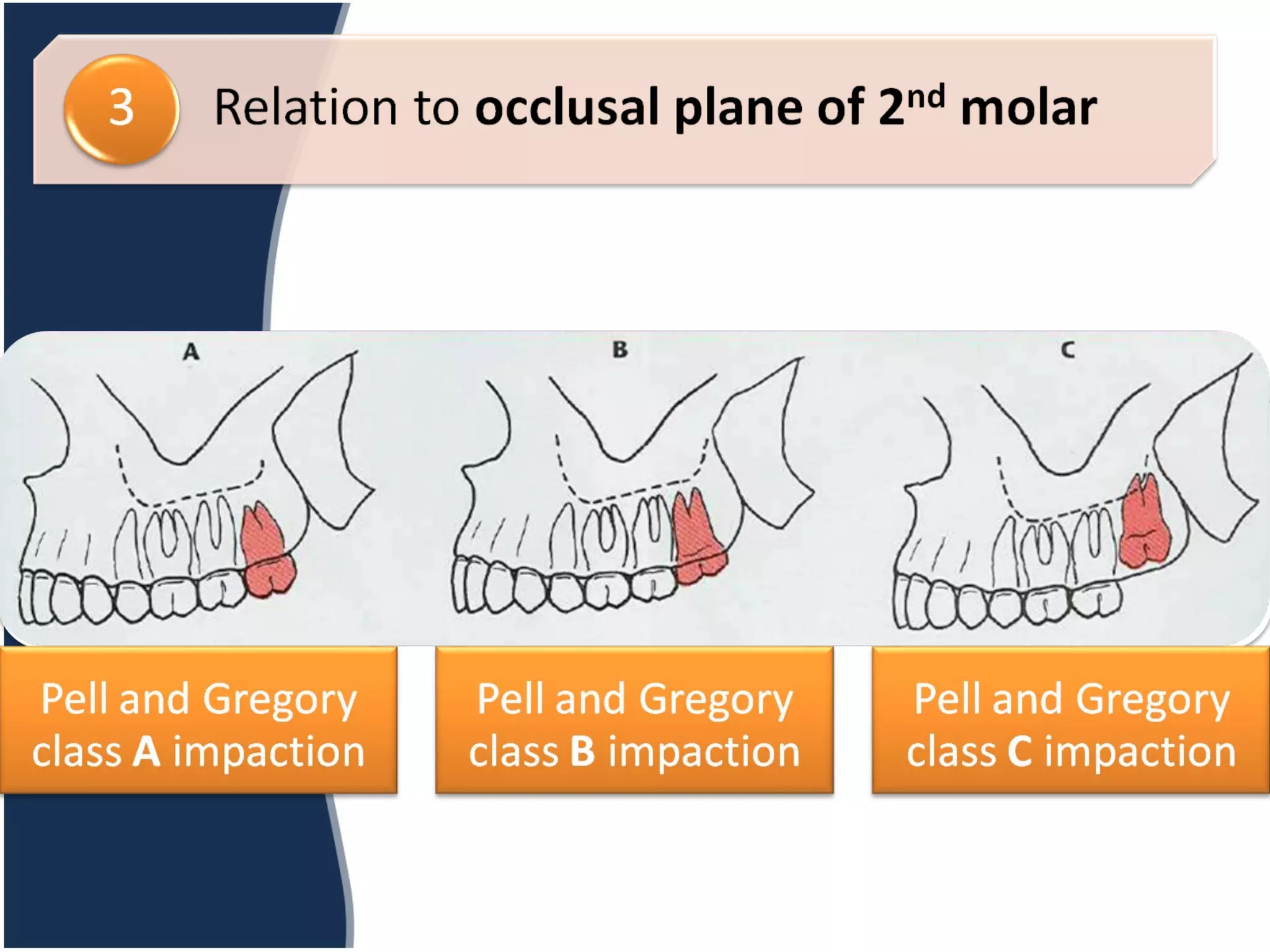
2. Common indications for surgical extraction include impacted teeth, excessive force required for non-impacted extractions, and prevention of cysts/tumors. Impacted teeth are classified based on their angle of impaction.
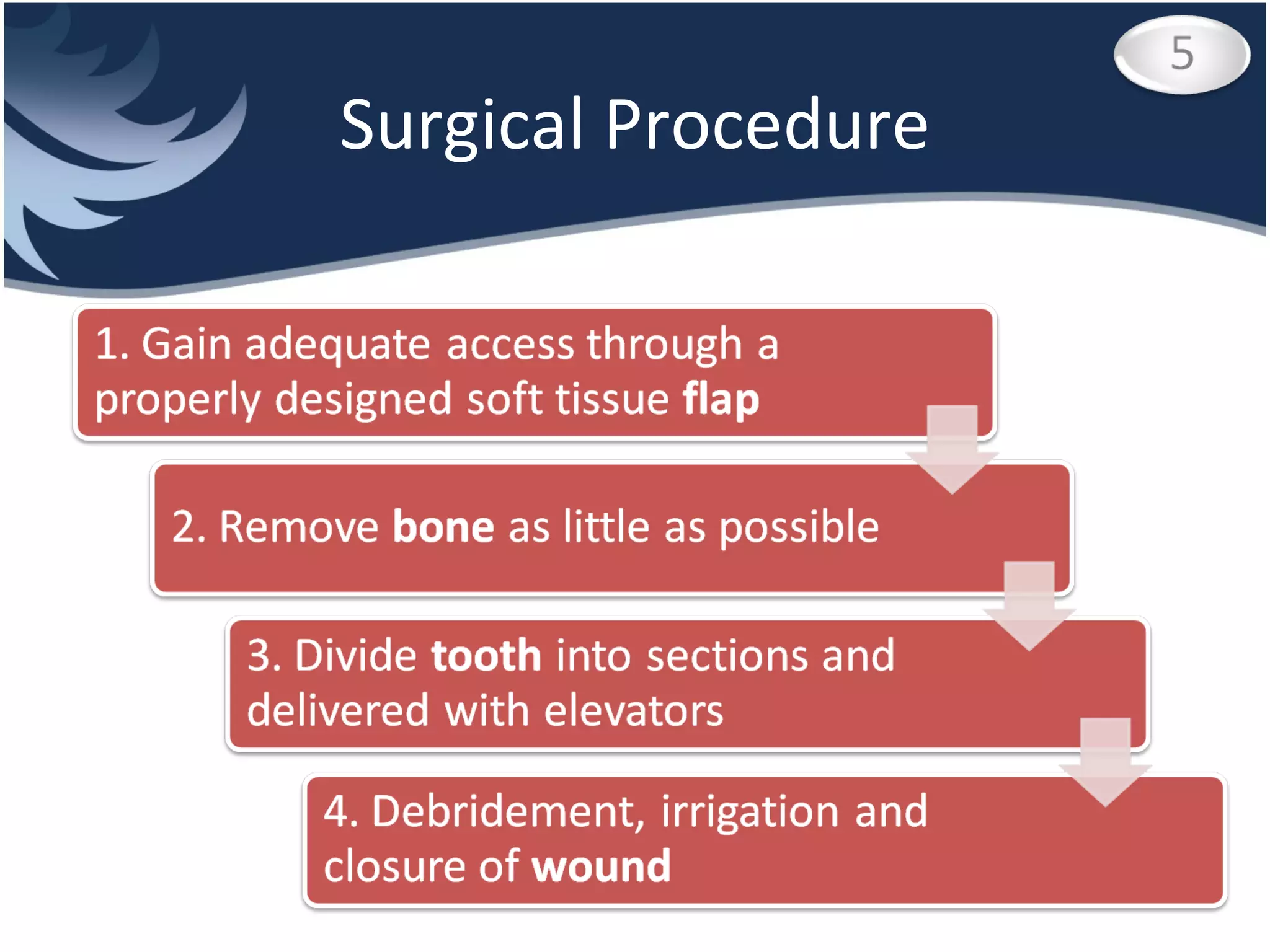
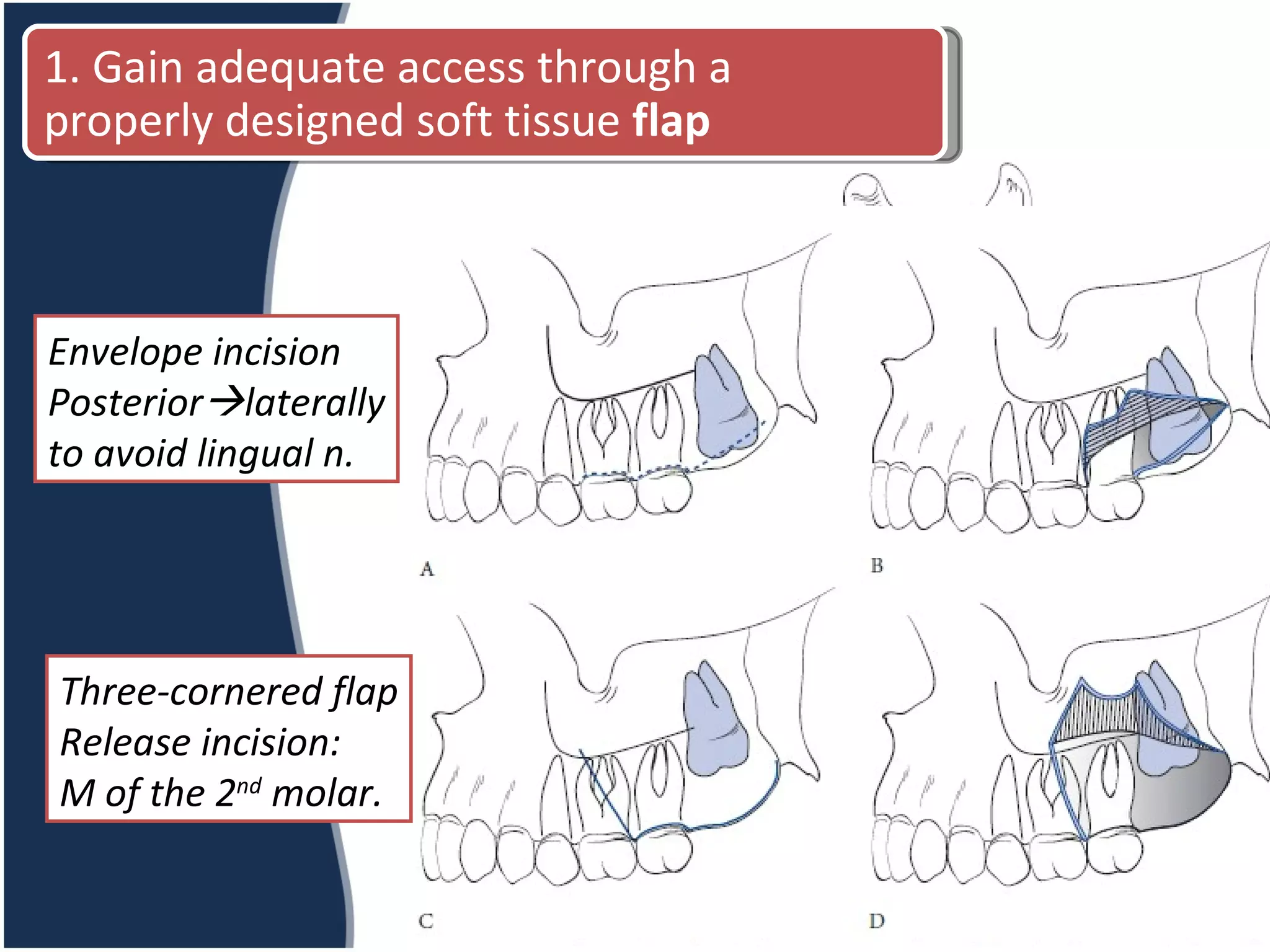
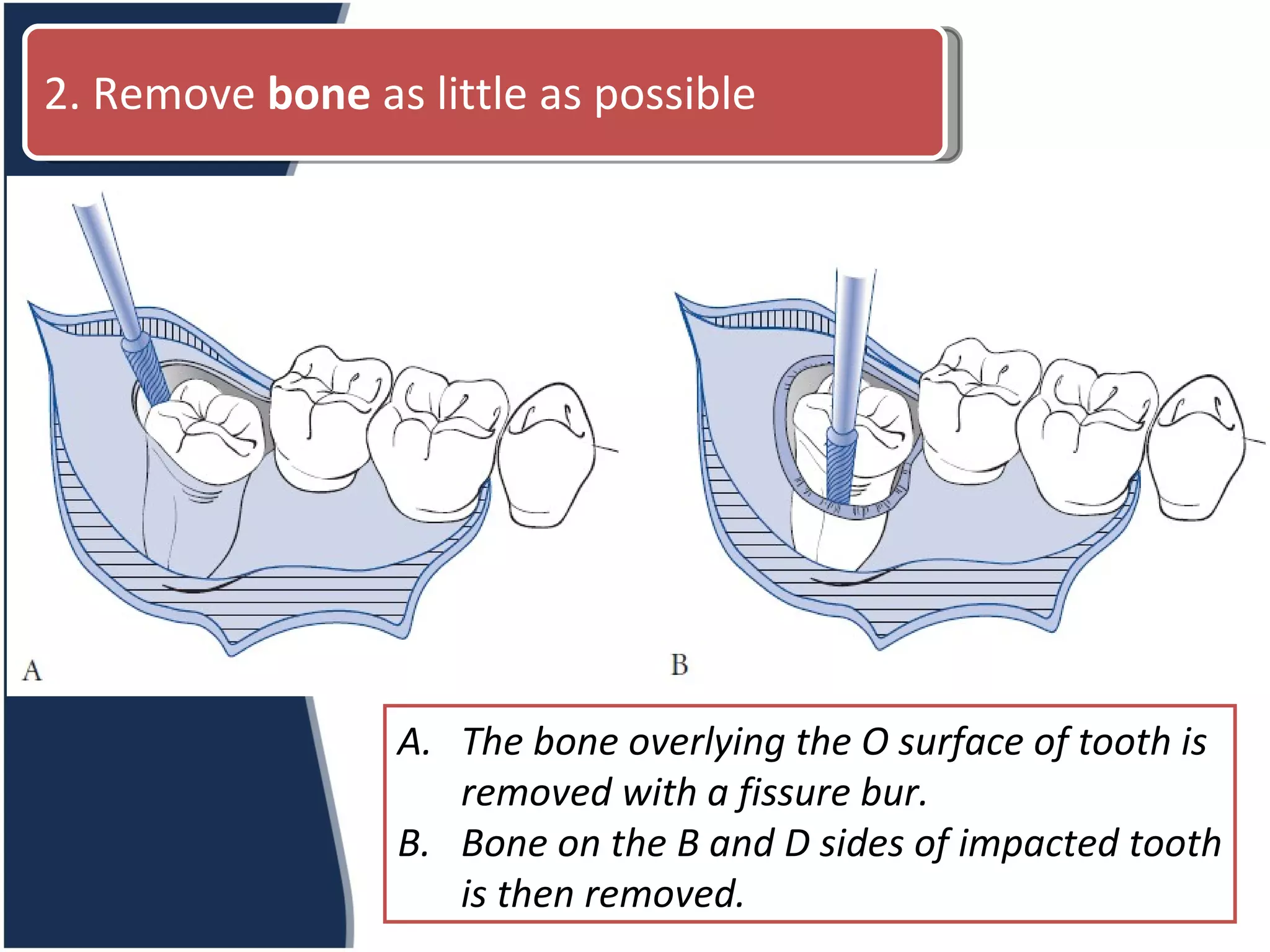
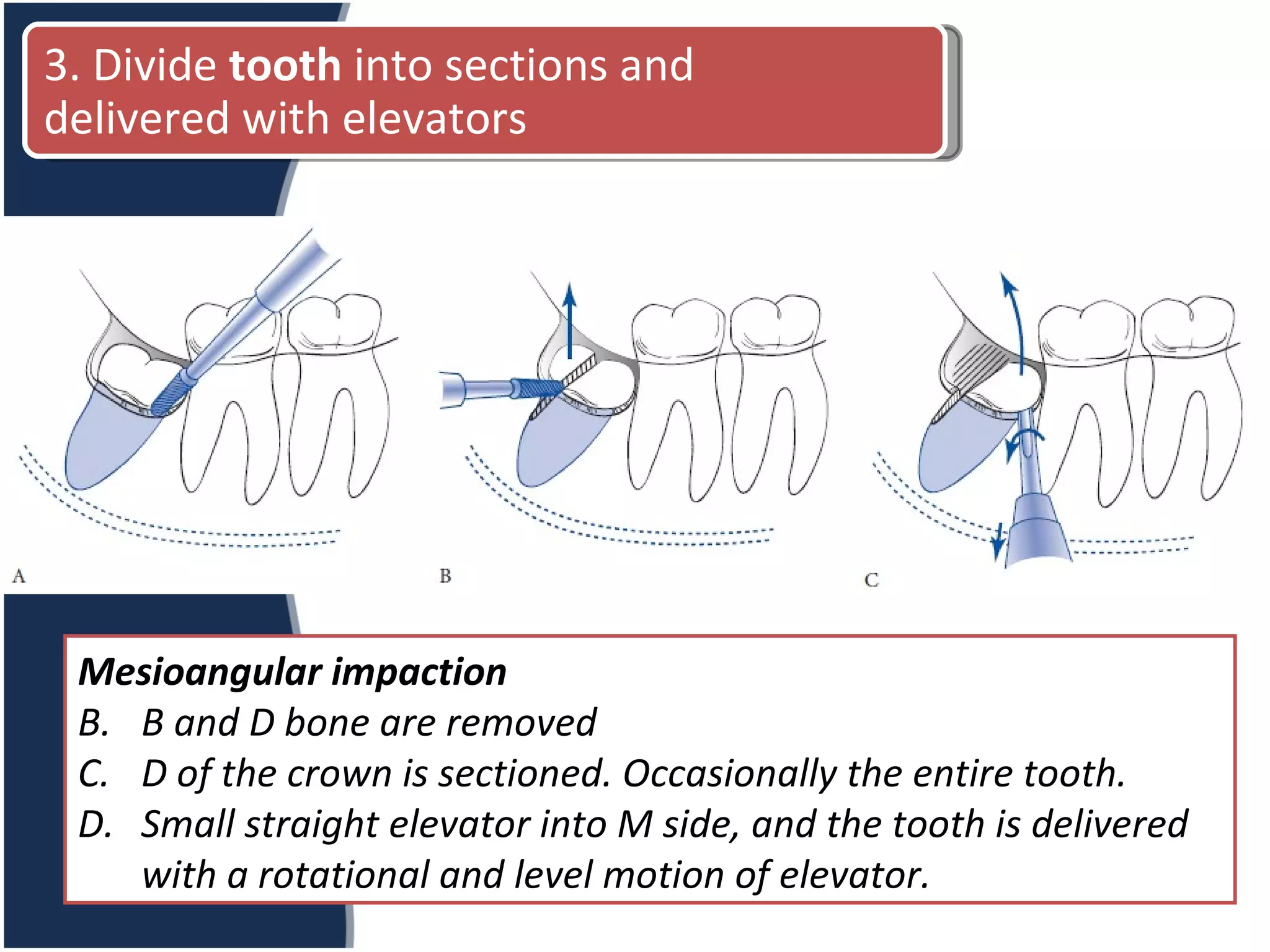
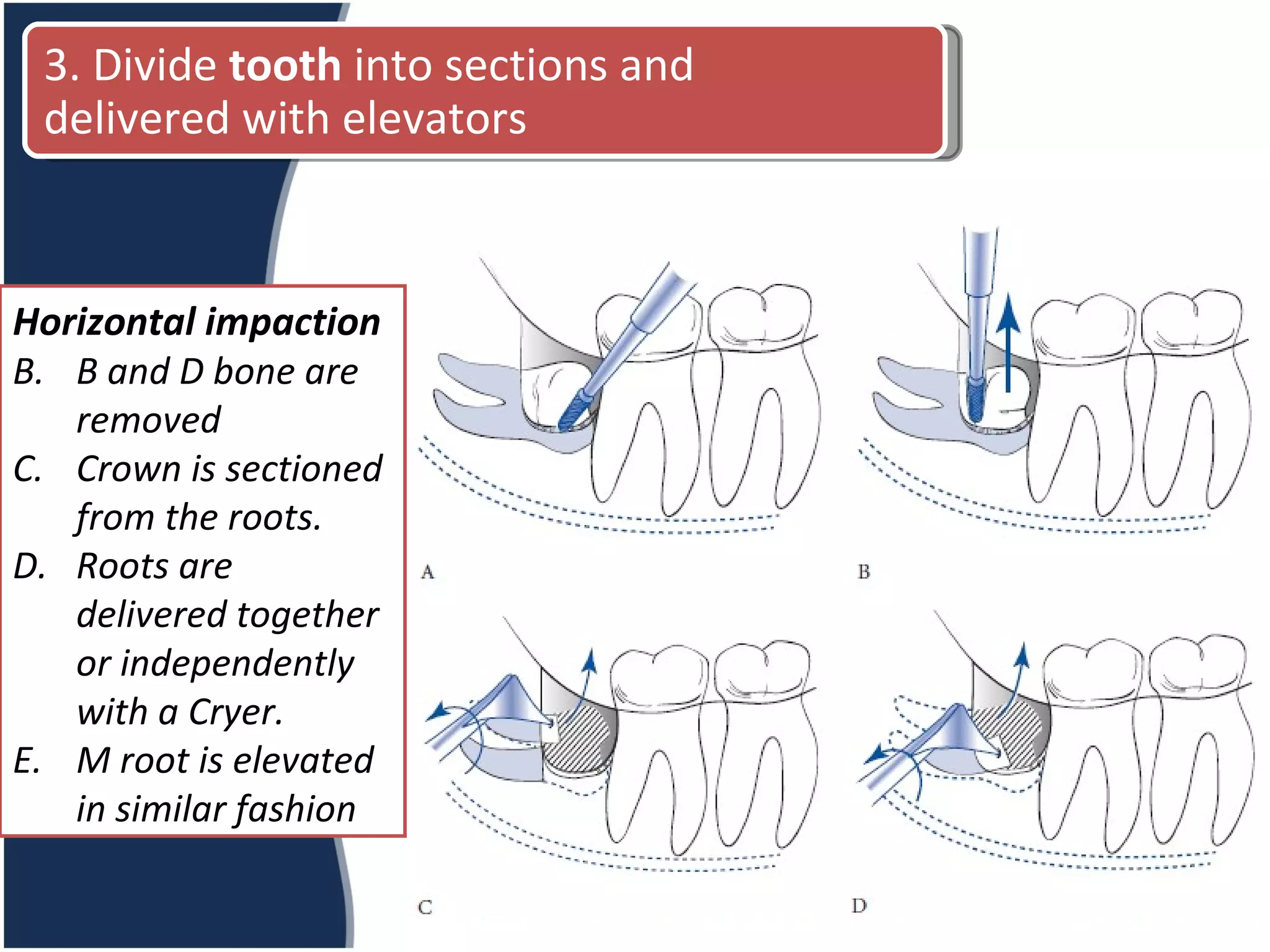
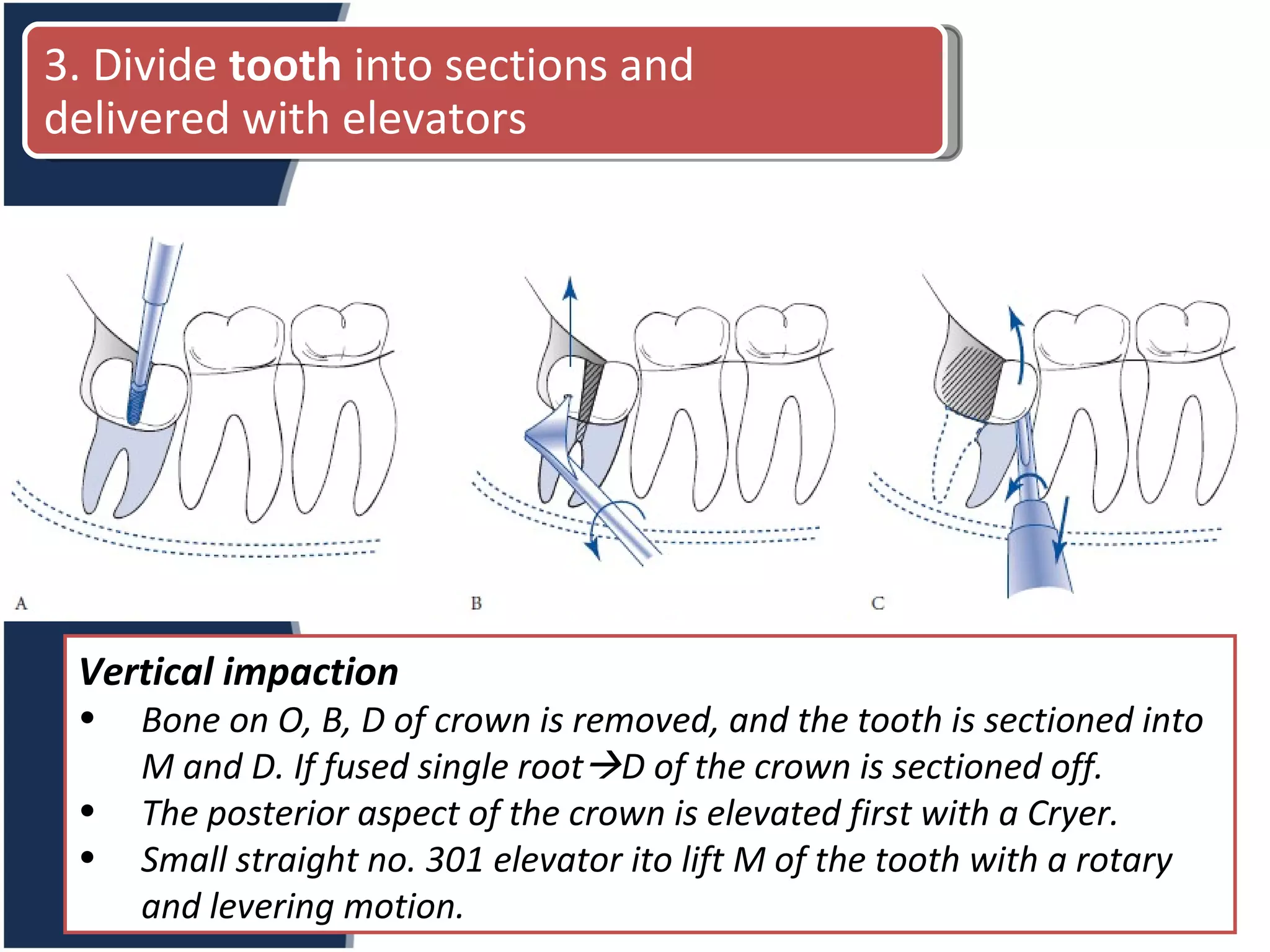
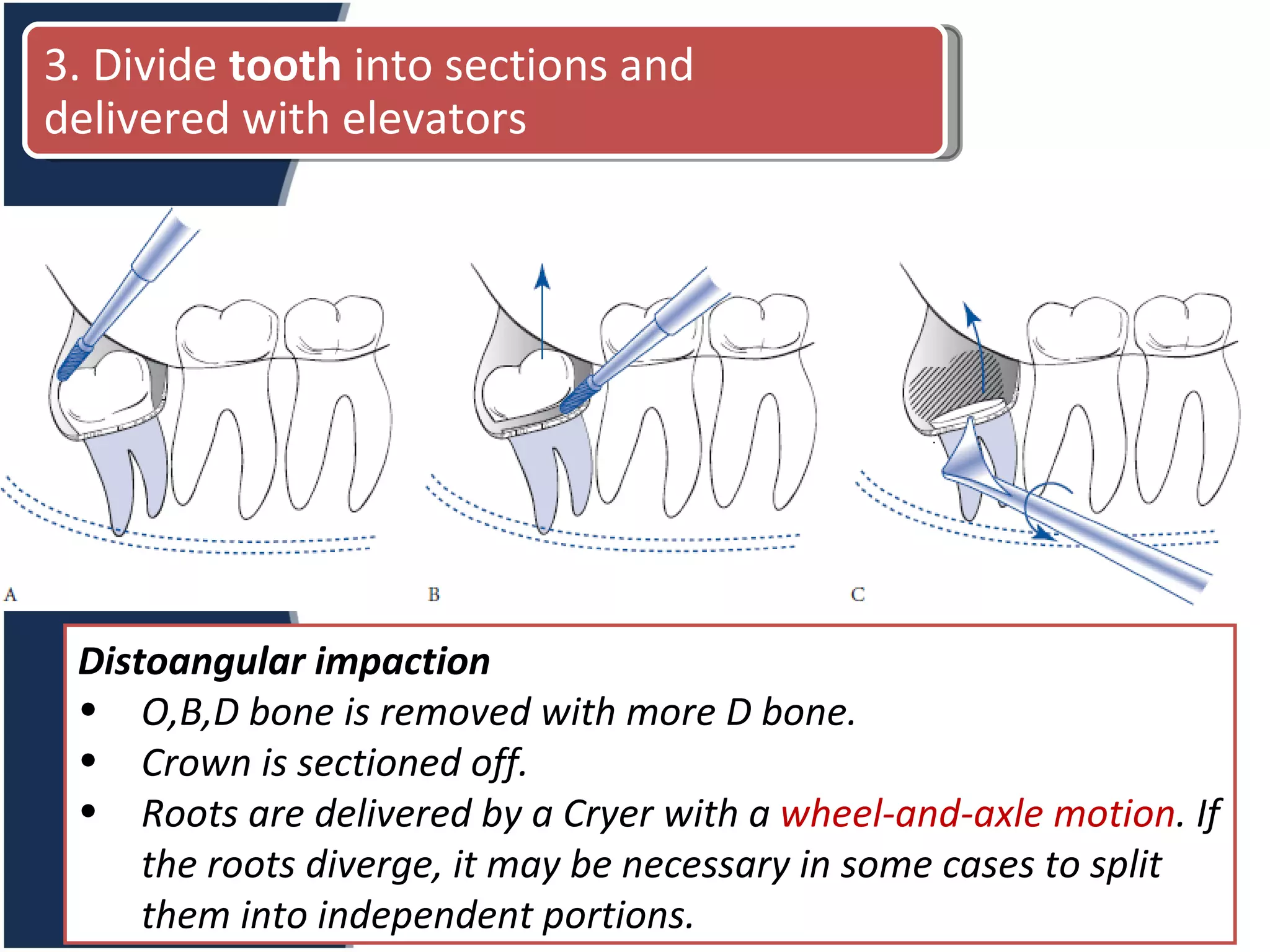
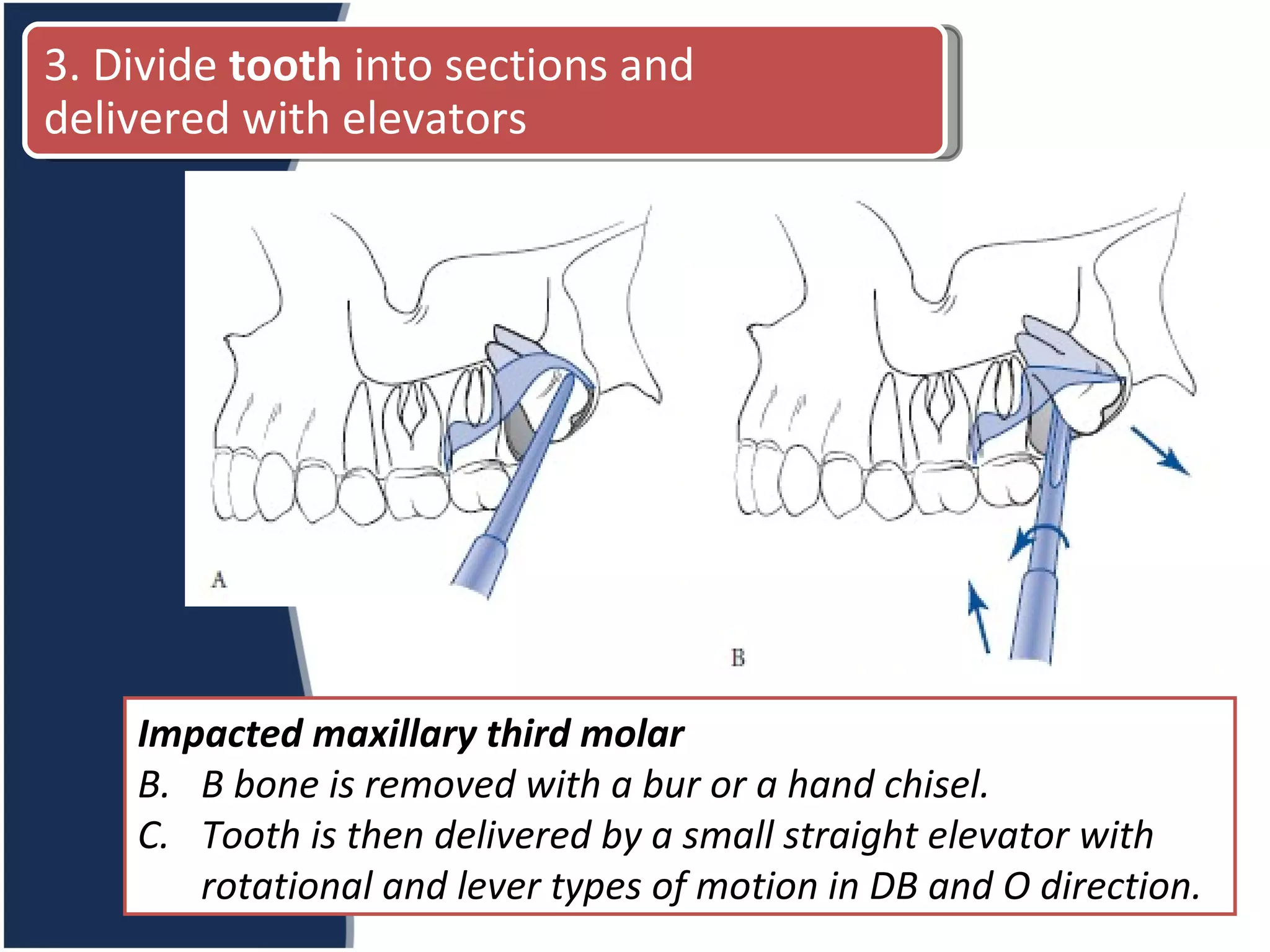
3. The surgical procedure involves raising soft tissue flaps, removing surrounding bone, sectioning and removing the tooth in segments using elevators. Postoperative care includes analgesics, antibiotics, and management of pain, swelling and potential complications like infection, nerve injury or dry socket.