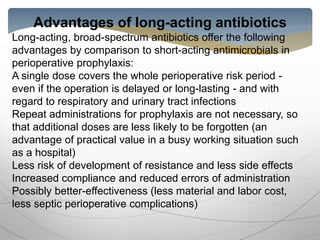
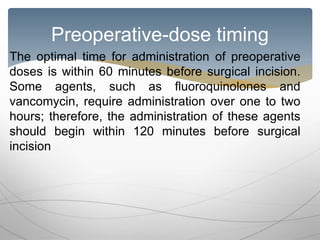
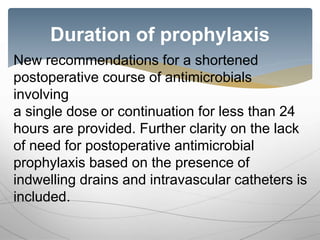
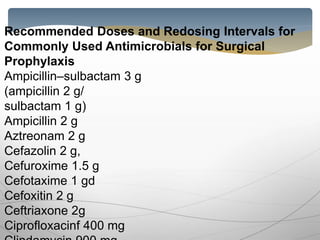
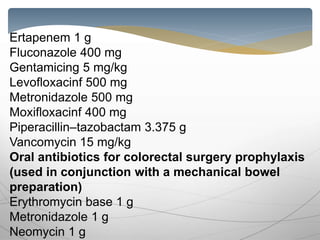
The document discusses antibiotic prophylaxis in surgery. It notes that while sterile techniques are used, surgeries can introduce bacteria which can cause infections. Antibiotics have been shown to effectively reduce postoperative infections. The appropriate choice of antibiotic is important, considering factors like the pathogens likely to be encountered, pharmacology, and ensuring adequate levels throughout the procedure. A single preoperative dose of a long-acting antibiotic that maintains effective levels throughout the surgery is preferred to minimize side effects and development of antibiotic resistance. Precise timing of administration is also important for effectiveness of prophylaxis.