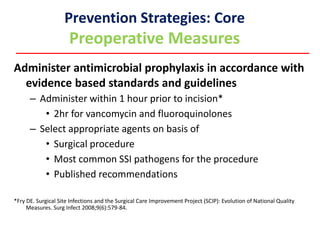
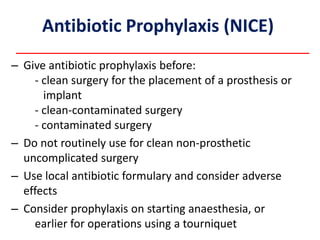
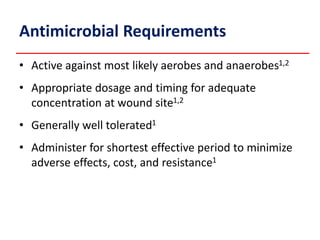
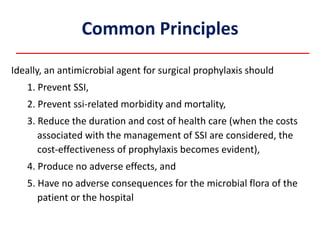
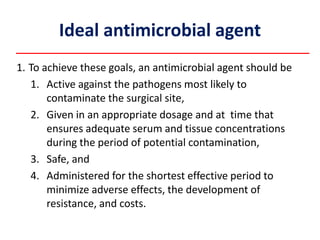
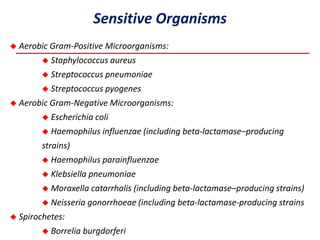
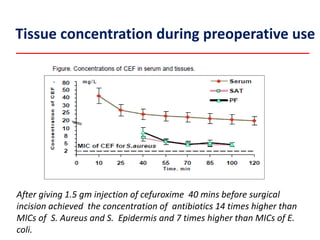
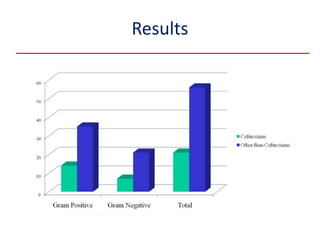
Cefuroxime is recommended for surgical antibiotic prophylaxis due to its broad-spectrum antibacterial activity against common pathogens. It achieves high concentrations in serum and tissues. Studies show cefuroxime is effective in reducing surgical site infections for procedures like hysterectomy and maxillofacial surgery when administered preoperatively. It has advantages of twice daily dosing, oral and IV formulations, and safety. Cefuroxime's broad spectrum and tissue penetration make it suitable for preventing postoperative infections from most bacteria encountered during surgery.