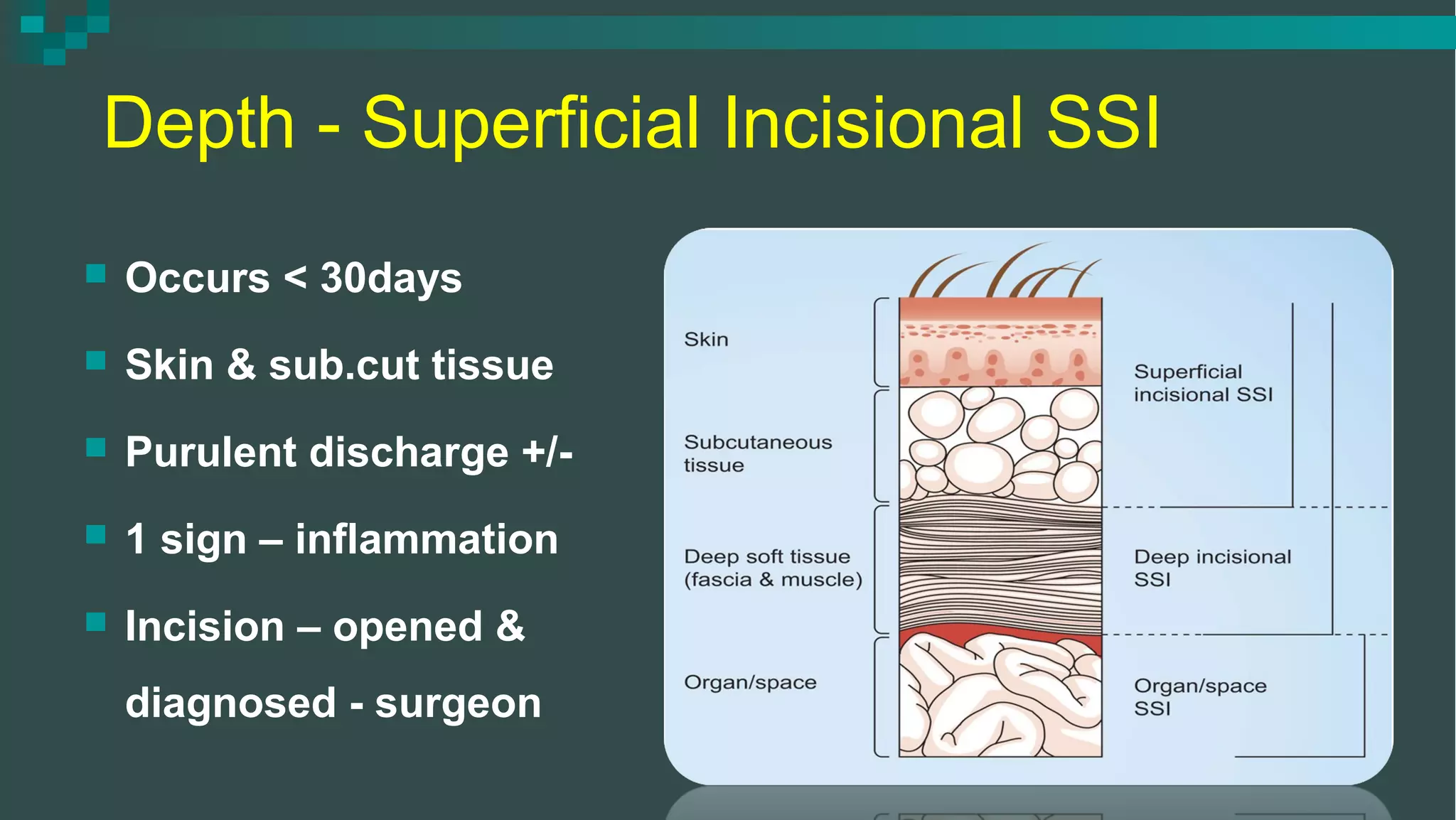
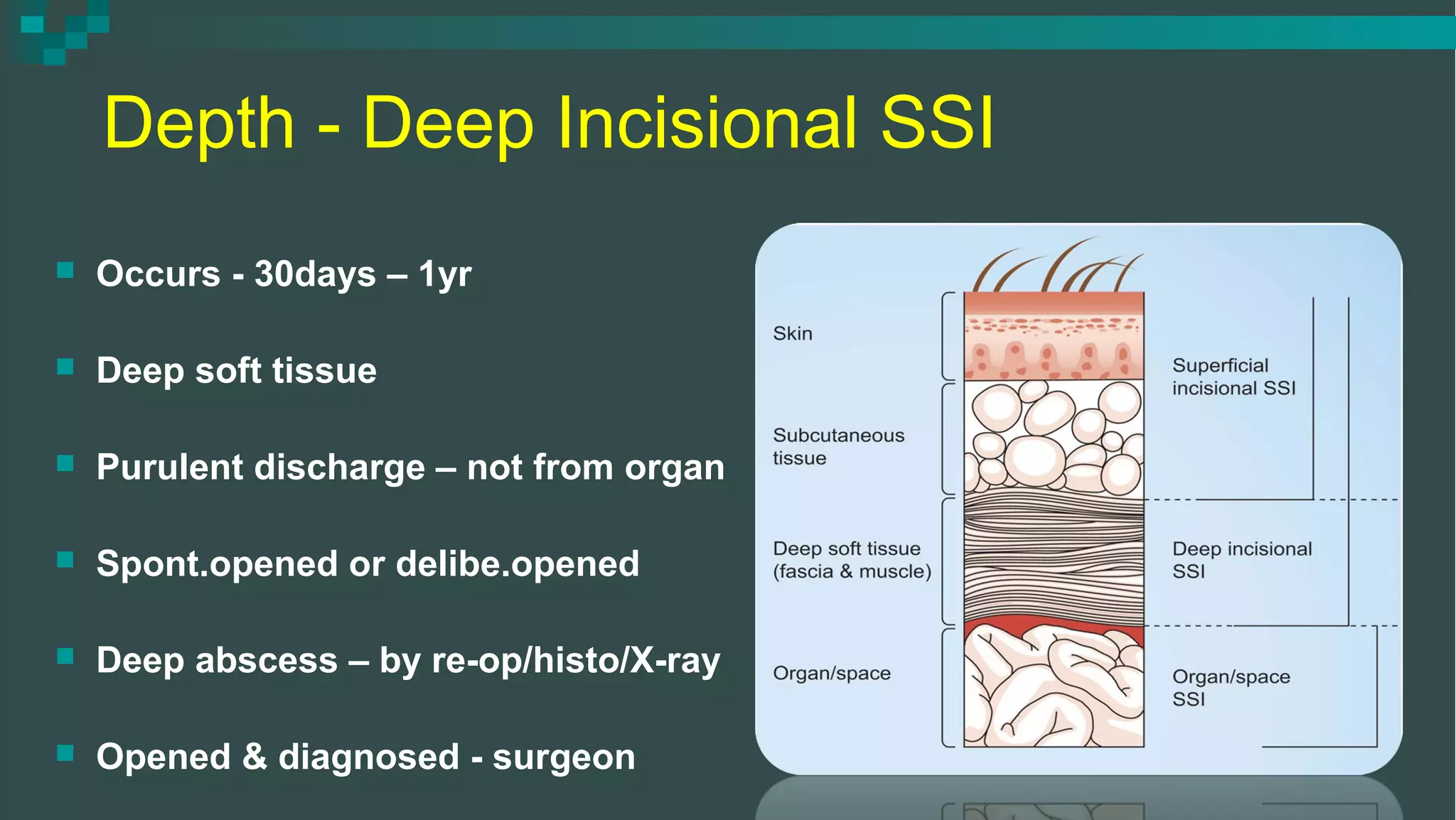
The document discusses surgical site infections (SSI), their definitions, etiology, and prevention strategies, emphasizing the challenge they pose in surgical practice and their association with increased healthcare costs. It outlines types of SSIs based on depth and occurrence, as well as risk factors, important definitions, and recommended preoperative measures and antibiotic prophylaxis. The document also details treatment options and specific antibiotic regimens tailored to various types of surgeries and pathogens.













![Depth - Organ / Space SSI
Occurs - 30days – 1yr
Involves – any part [organ/space]
Purulent discharge – drain
Organisms – isolated
Deep abscess – direct & re-op /
histology / X-ray
Opened & diagnosed - surgeon](https://image.slidesharecdn.com/ssi-dr-151104081151-lva1-app6891/75/Surgical-Site-Infection-18-2048.jpg)