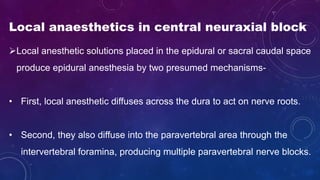
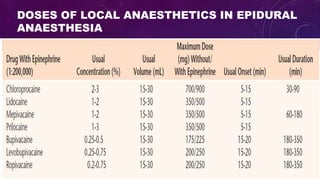
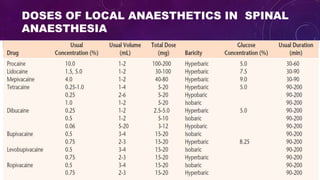
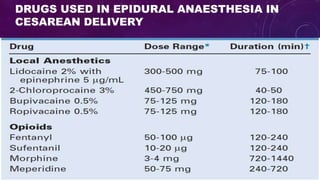
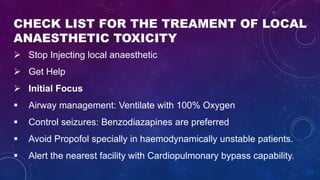
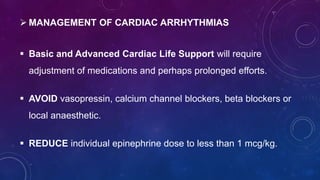
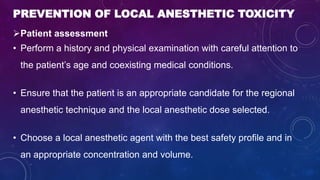
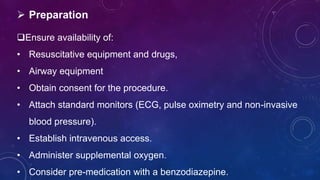
This document summarizes information about local anesthetics used in central neuraxial blocks and their toxicity. It discusses how local anesthetics work, the drugs and doses used in epidural and spinal anesthesia, risks of local anesthetic systemic toxicity, prevention methods, and treatment of toxicity. Signs and symptoms of toxicity are outlined for the central nervous and cardiovascular systems. Risk factors, complications like methemoglobinemia, and neural toxicity are also reviewed.