1) The document provides information on the evaluation and management of bleeding per rectum (BPR). It discusses the history, physical exam, differential diagnoses, investigations and treatment options for common causes of BPR.
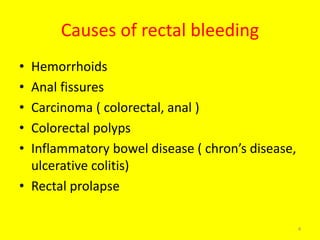
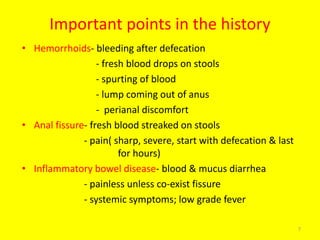
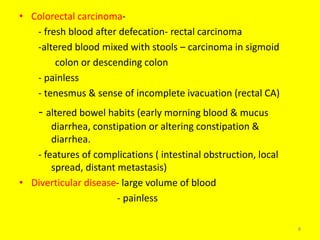
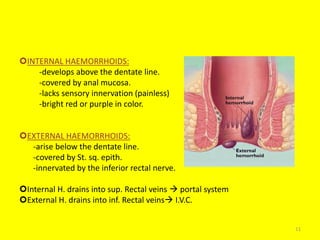
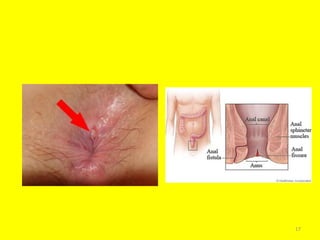
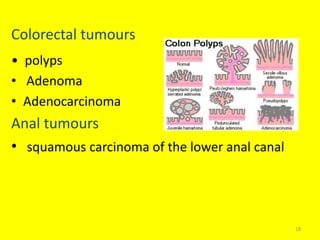
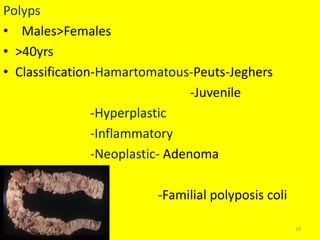
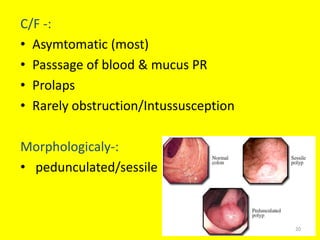
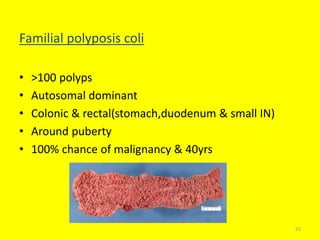
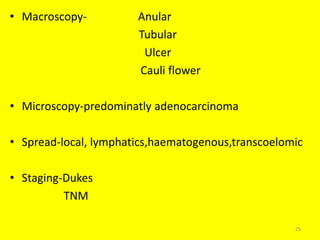
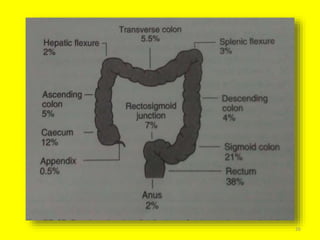
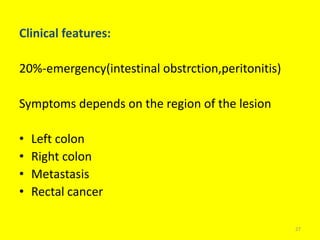
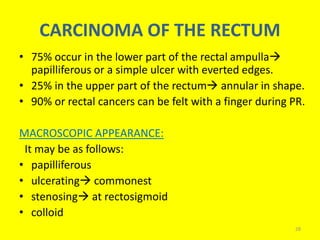
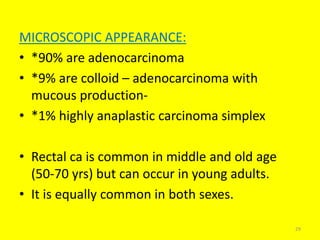
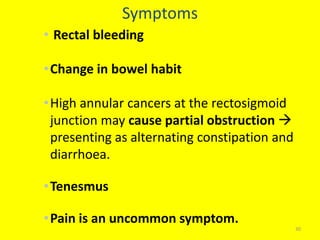
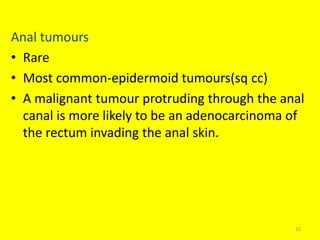
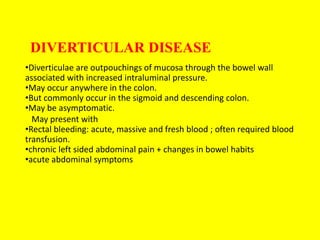
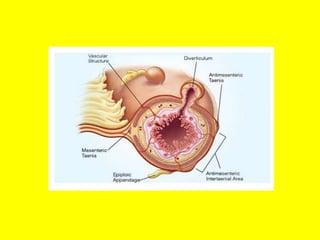
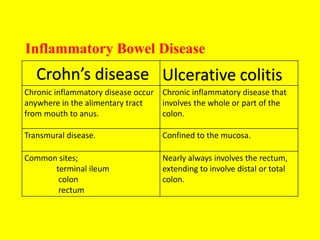
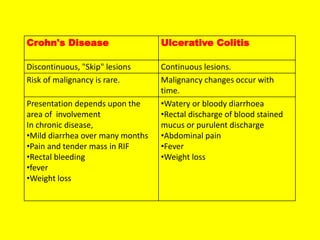
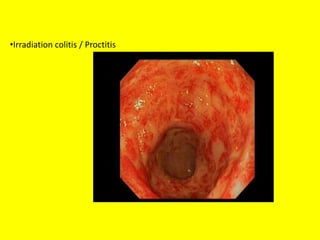
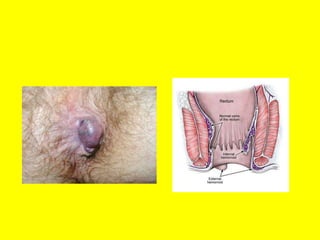
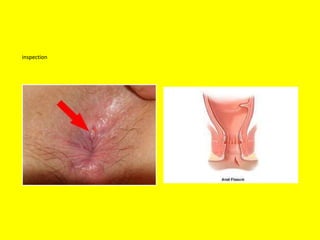
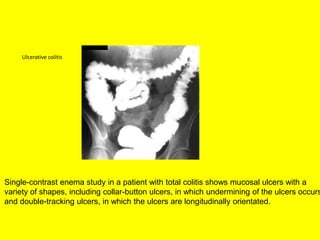
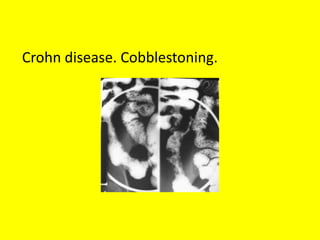
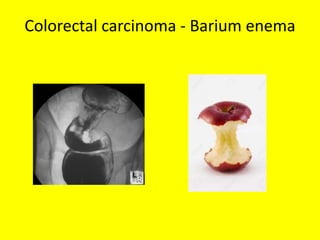
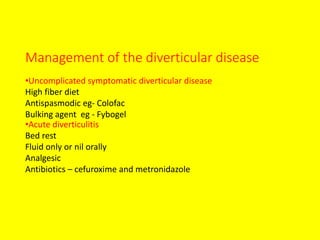
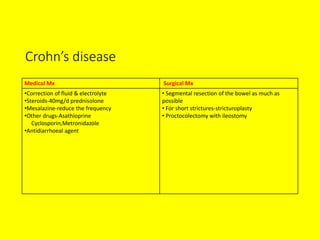
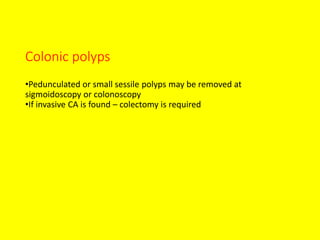
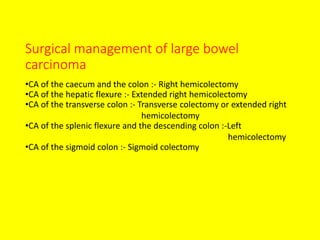
2) Common causes of BPR include hemorrhoids, anal fissures, colorectal polyps, inflammatory bowel disease, diverticular disease, and colorectal cancers. The history can help determine if the bleeding is from distal or proximal lesions.
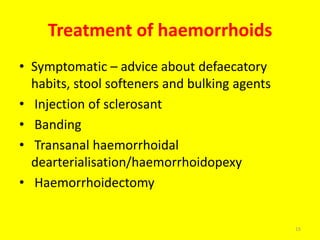
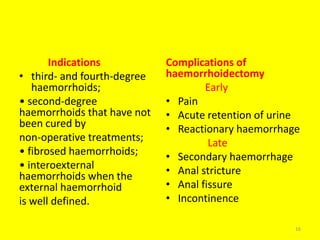
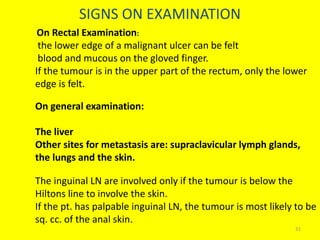
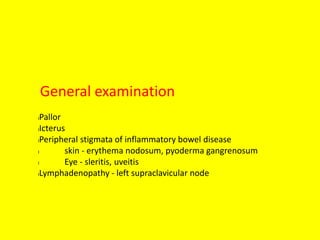
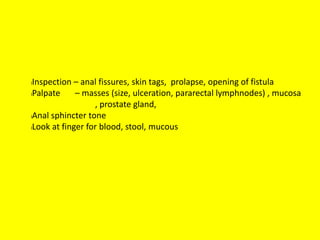
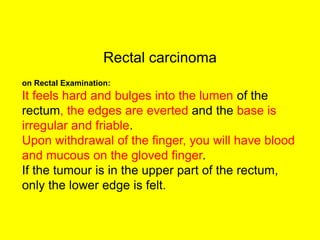
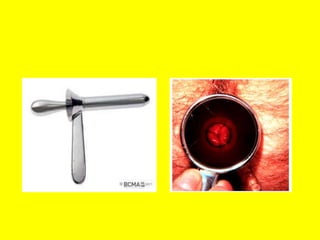
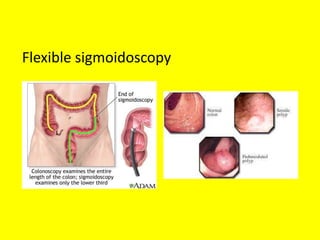
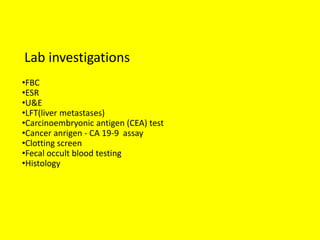
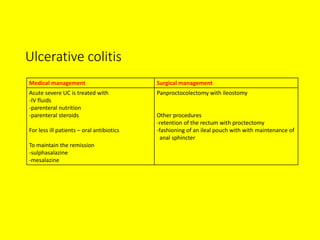
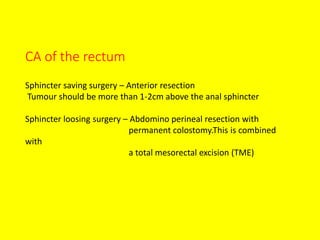
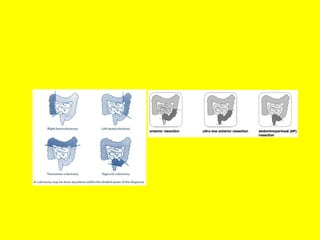
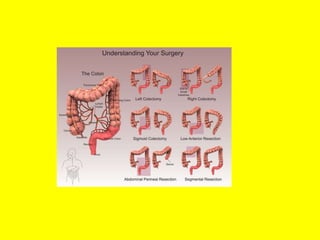
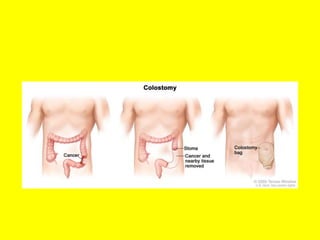
3) Physical exam involves digital rectal exam to feel for masses or other abnormalities. Initial investigations include labs, endoscopy, and imaging. Treatment depends on the underlying cause but may include medications, procedures like banding or surgery.