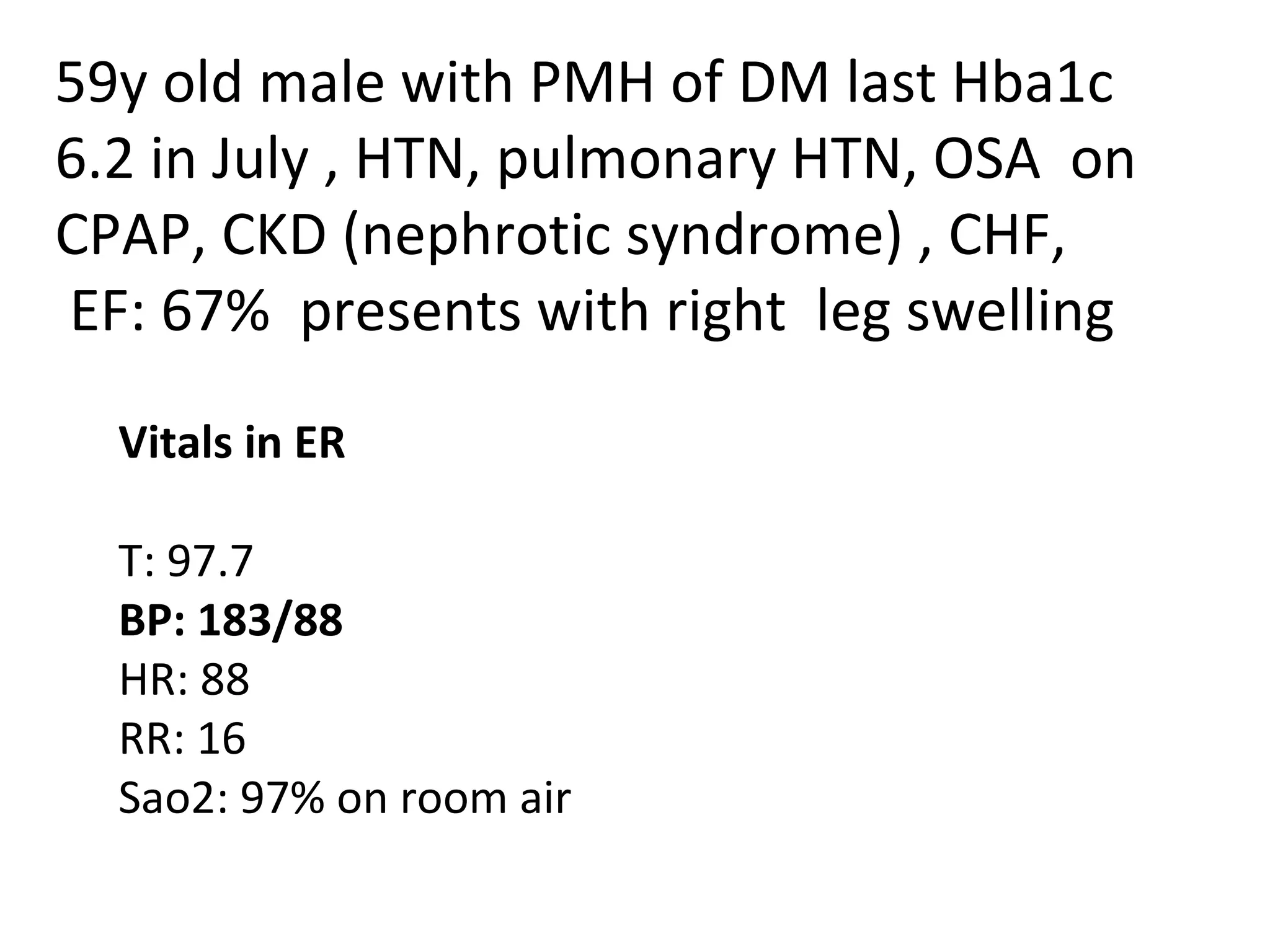
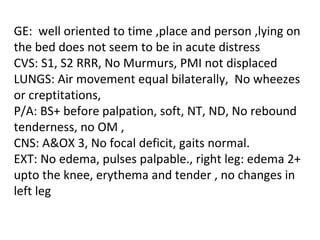
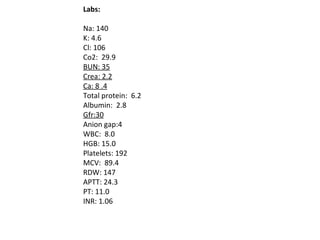
This document summarizes the evaluation and treatment of a 59-year-old man presenting with right leg swelling and edema. It notes his medical history including diabetes, hypertension, pulmonary hypertension, sleep apnea, chronic kidney disease, and congestive heart failure. It discusses diagnostic testing performed, including a positive D-dimer and imaging, and treatment options for deep vein thrombosis including anticoagulant medications like warfarin, heparin, and fondaparinux as well as interventional procedures like IVC filters and thrombolytic therapy in certain situations.
![TREATMENT To prevent recurrent VTE, To prevent consequences of VTE (i.e., post-phlebitic syndrome [i.e., pain, edema, and ulceration], pulmonary arterial hypertension, and death), and To prevent complications of therapy (e.g., bleeding and HIT).](https://image.slidesharecdn.com/presentationaug2011-110731175926-phpapp01/85/Presentationaug2011-8-320.jpg)