1. Deep vein thrombosis (DVT) and pulmonary embolism (PE) are manifestations of venous thromboembolism (VTE) which occurs due to Virchow's triad of stasis, hypercoagulability, and endothelial injury.
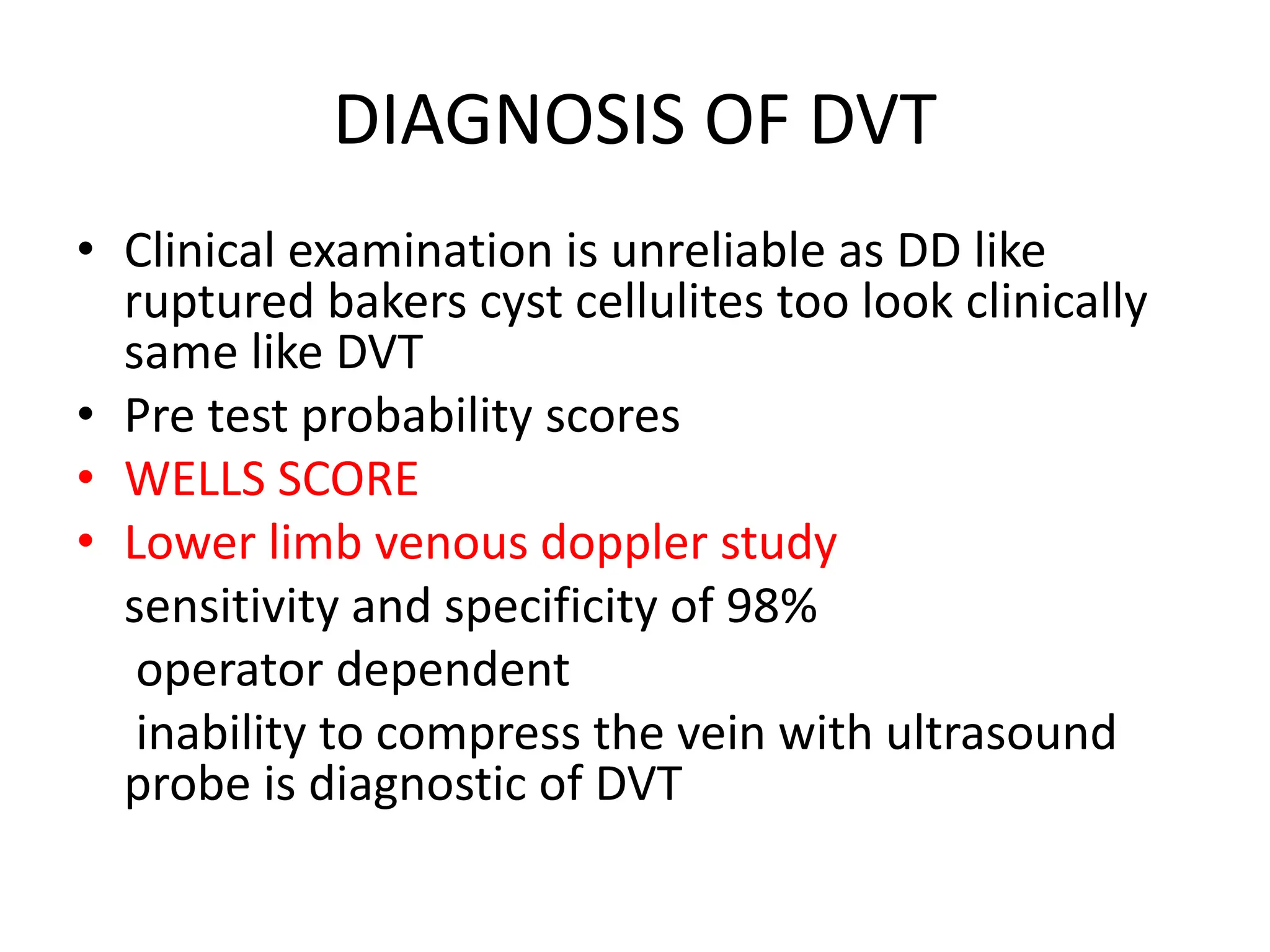
2. The document presents several case studies demonstrating the diagnosis and management of DVT and PE. Clinical features, diagnostic testing including Doppler ultrasound, CT pulmonary angiogram, and echocardiogram are discussed.
3. Treatment involves anticoagulation with heparin, low molecular weight heparin, or novel oral anticoagulants initially followed by vitamin K antagonists. Thrombolytic therapy may be used in massive PE