1) A study compared the yield of CT pulmonary angiograms (CTPAs) for patients with pulmonary embolism (PE) when clinicians overrode clinical decision support (CDS) guidelines versus adhering to them.
2) The override group had a lower yield of PE detection (4.2% vs 11.2%) and 51.3% lower odds of acute PE compared to the adherent group.
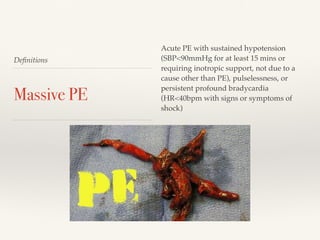
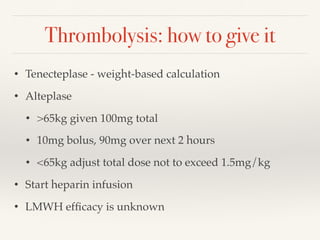
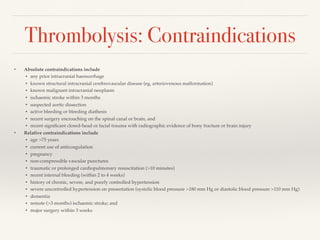
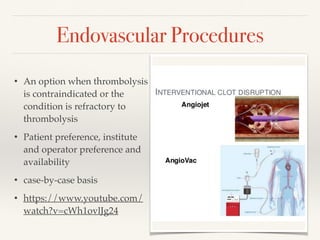
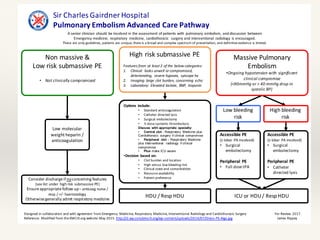
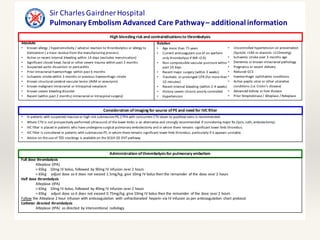
3) Guidelines for PE management include anticoagulation, thrombolysis, catheter-directed thrombolysis, surgical embolectomy, and consideration of inferior vena cava filters depending on the risk level and characteristics of the patient's PE.