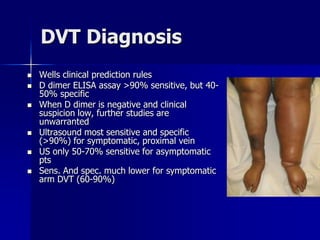
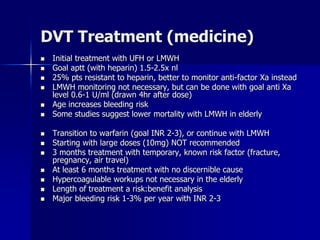
This document provides a historical overview of the diagnosis and treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE). It discusses key discoveries and studies that advanced the understanding and management of these conditions, such as Virchow identifying PE in 1846, studies in the 1960s establishing the use of heparin to prevent DVT and fatal PE after surgery, and randomized controlled trials in the 1990s comparing heparin/warfarin to heparin/warfarin plus inferior vena cava filters for DVT treatment. The document also reviews current diagnostic methods and medical and interventional treatment options for DVT and PE.






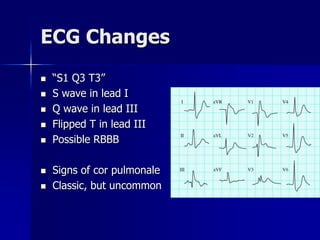
![Arterial Blood Gas
Hyperventilation leads to low pCO2
Difficulty in oxygenation
Alveolar-arterial gradient may be
elevated (80% of cases)
A-a O2 Gradient = [ (FiO2) *
(Atmospheric Pressure - H2O
Pressure) - (PaCO2/0.8) ] -
PaO2 from ABG
Nl Gradient Estimate = (Age/4) + 4](https://image.slidesharecdn.com/rtcdvtandpe-230915142910-4a3e1e88/85/RTC-DVT-AND-PE-ppt-11-320.jpg)