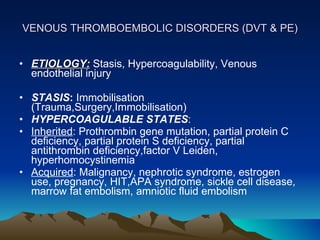
1. A 35-year-old man presented with acute onset of breathlessness and was found to have pulmonary thromboembolism and deficiencies in protein C and protein S without evidence of deep vein thrombosis.
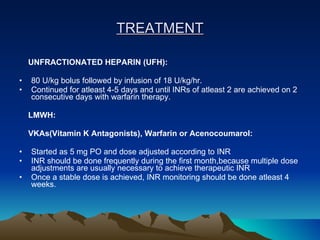
2. He was treated with supportive measures, heparin, acenocoumarol, and supplements but developed massive hemoptysis and succumbed to his illness despite intensive care.
3. The case report discusses evaluation, treatment, and long-term management of venous thromboembolism and highlights complications that can arise.

























![INVASIVE SPECIAL THERAPIES IVC FILTERS: 1] Acute DVT states in which there is absolute contraindication to anticoagulation 2] Recurrent thromboembolic episodes CATHETER EMBOLECTOMY SURGICAL EMBOLECTOMY](https://image.slidesharecdn.com/hemoptysis2-091013115341-phpapp01/85/Case-2-Pulmonary-Thromboembolism-31-320.jpg)