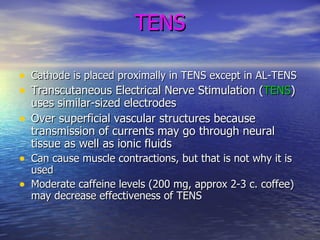
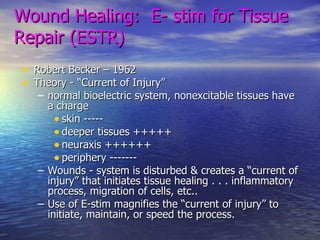
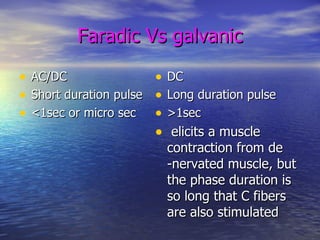
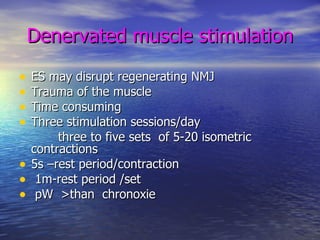
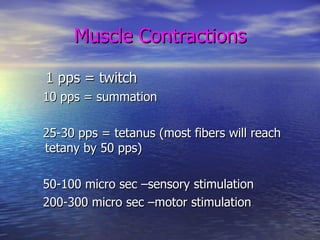
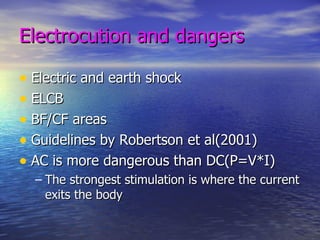
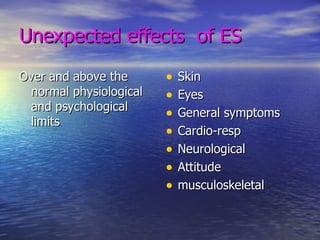
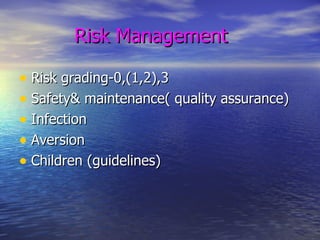
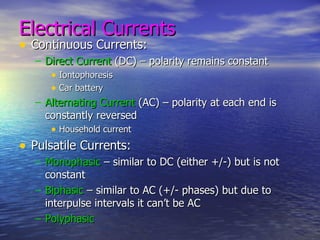
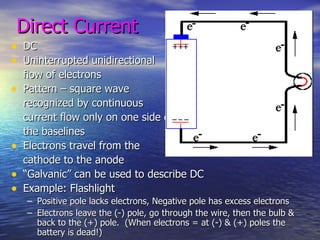
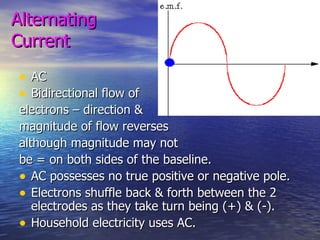
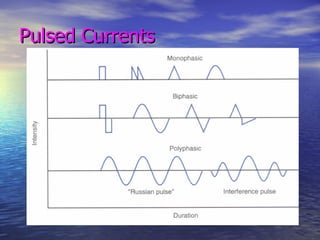
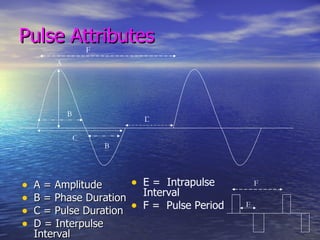
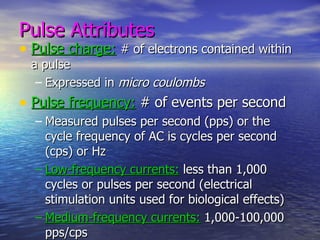
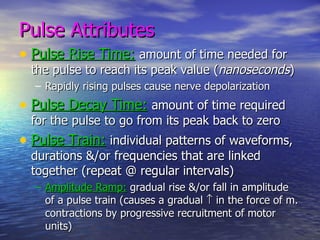
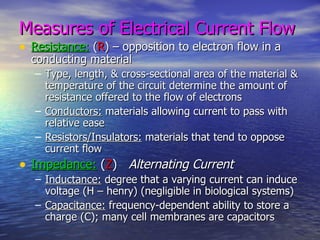
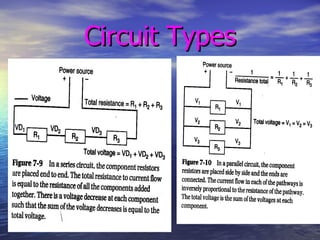
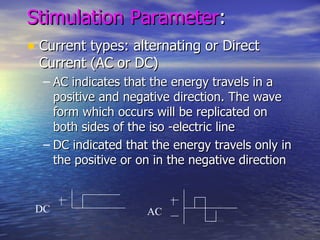
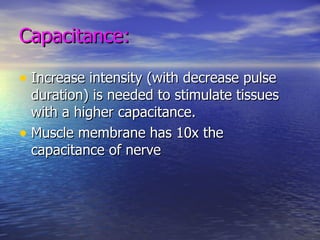
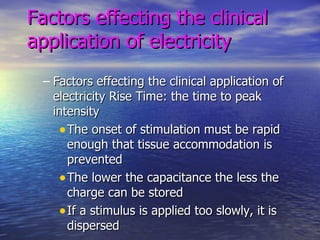
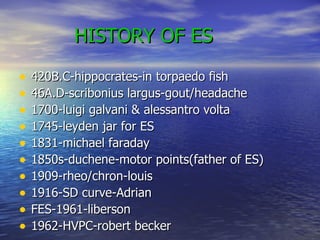
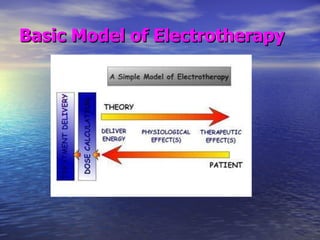
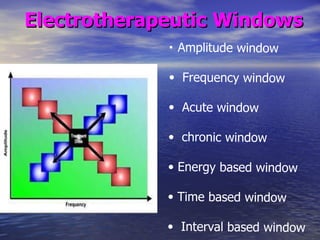
The document discusses various types of electrical currents used in electrical stimulation (ES), including direct current (DC), alternating current (AC), and pulsed currents. It describes attributes of pulses used in ES like amplitude, frequency, pulse duration, and duty cycle. It discusses factors that influence the clinical application of ES like stimulation parameters, tissue properties, and the history of ES. The document provides an overview of electrical concepts and principles relevant to understanding ES.



![Van Tulder et al . [ 1 ] specify that "strong evidence" is provided by multiple high quality randomised trials with consistent findings, "moderate evidence" is provided by consistent findings in multiple low quality trials, and "limited or conflicting evidence" is provided by only one randomised trial or by inconsistent findings “ No evidence”one low quality RCT/CCT](https://image.slidesharecdn.com/presentation21-4-11electrotherapy-120201082257-phpapp01/85/Presentation-21-4-11electrotherapy-44-320.jpg)