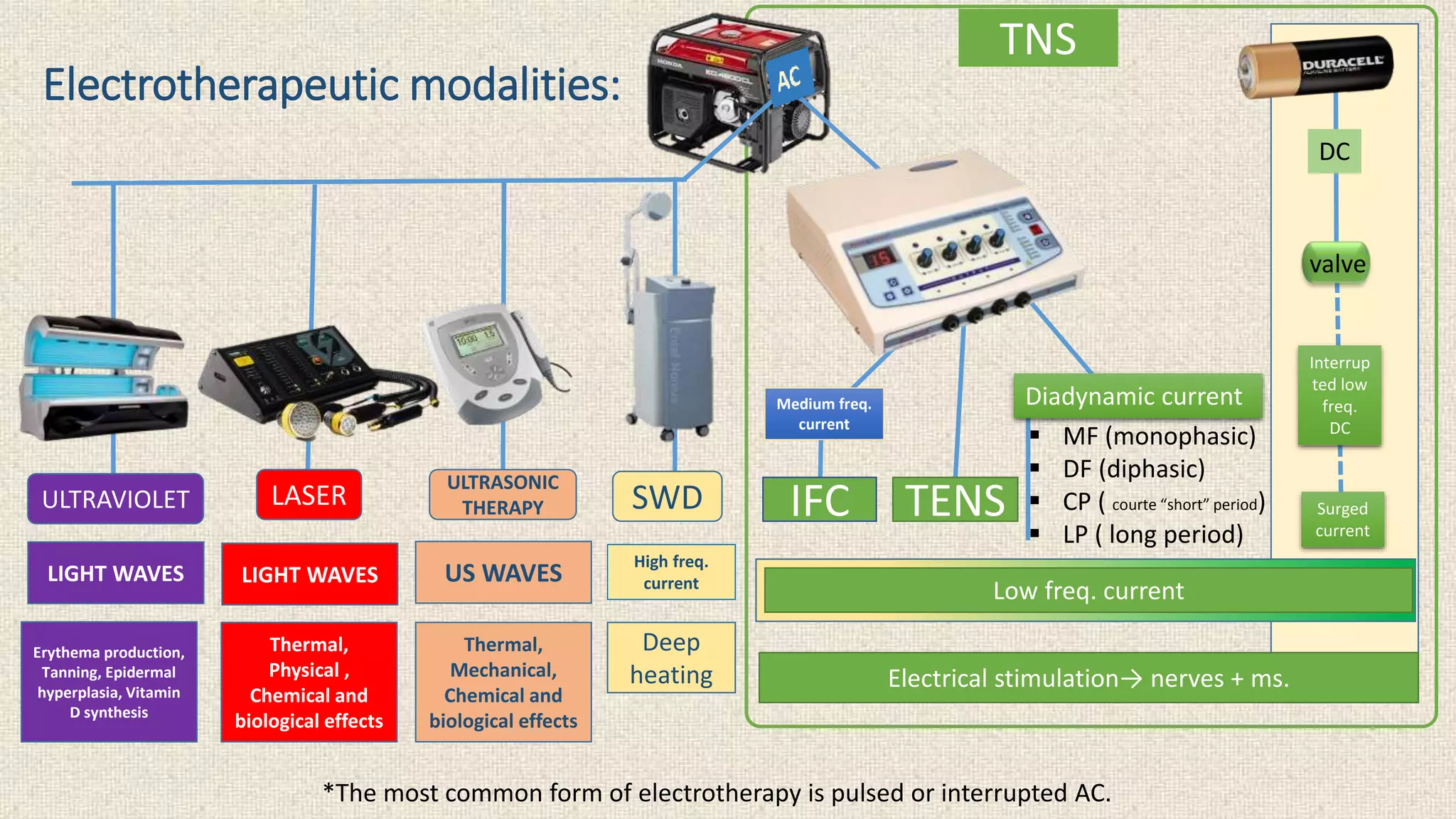
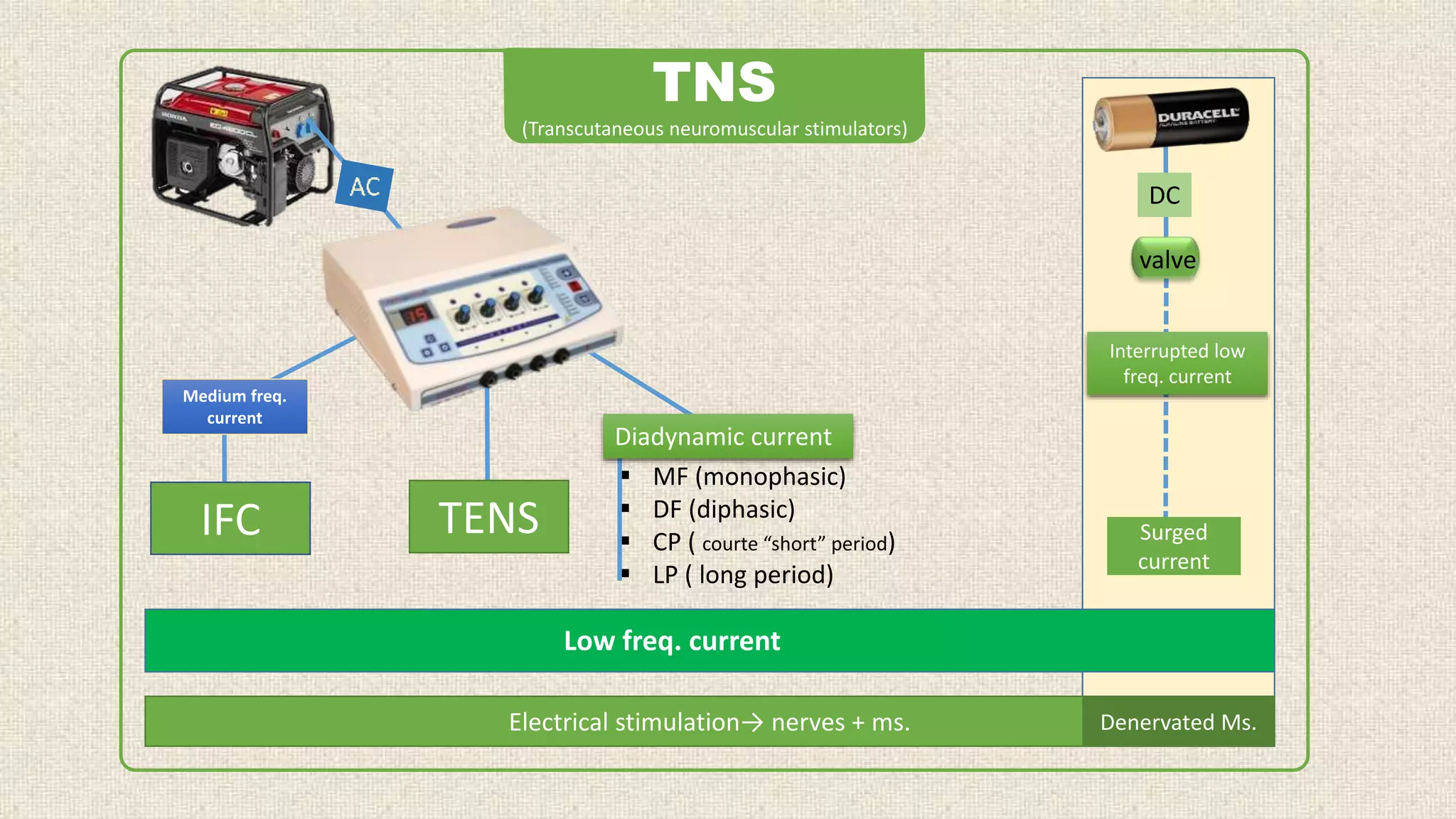
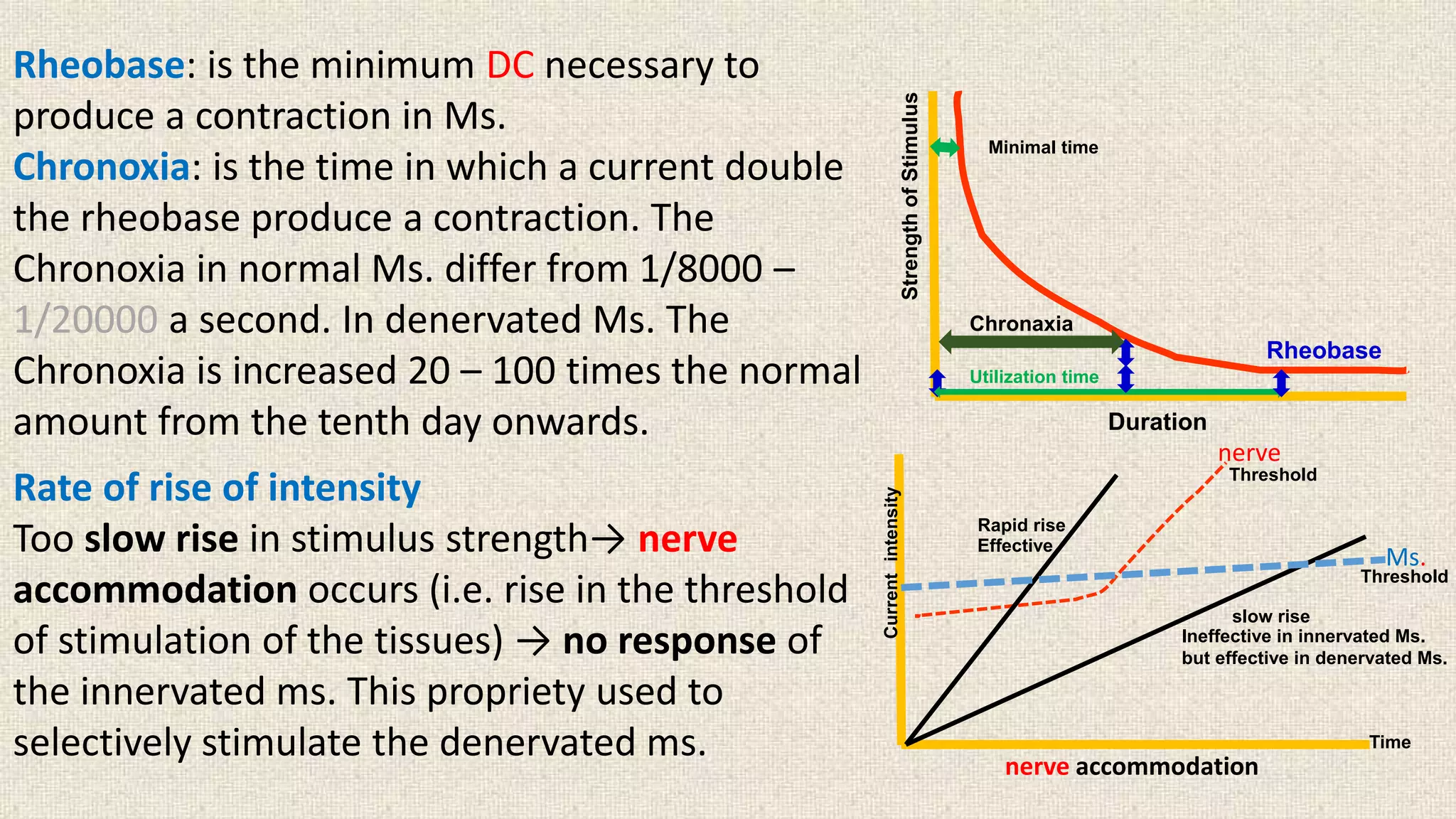
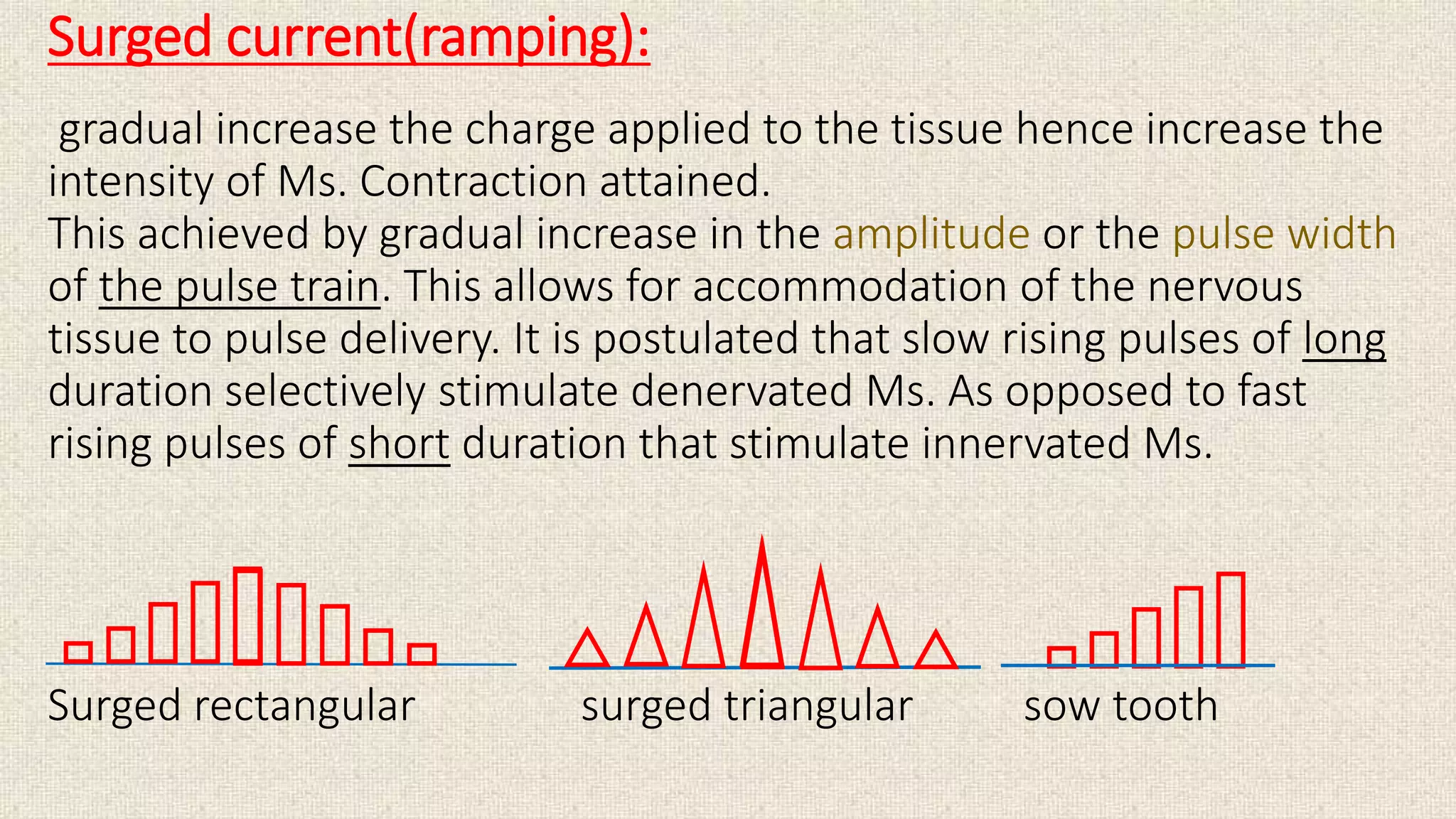
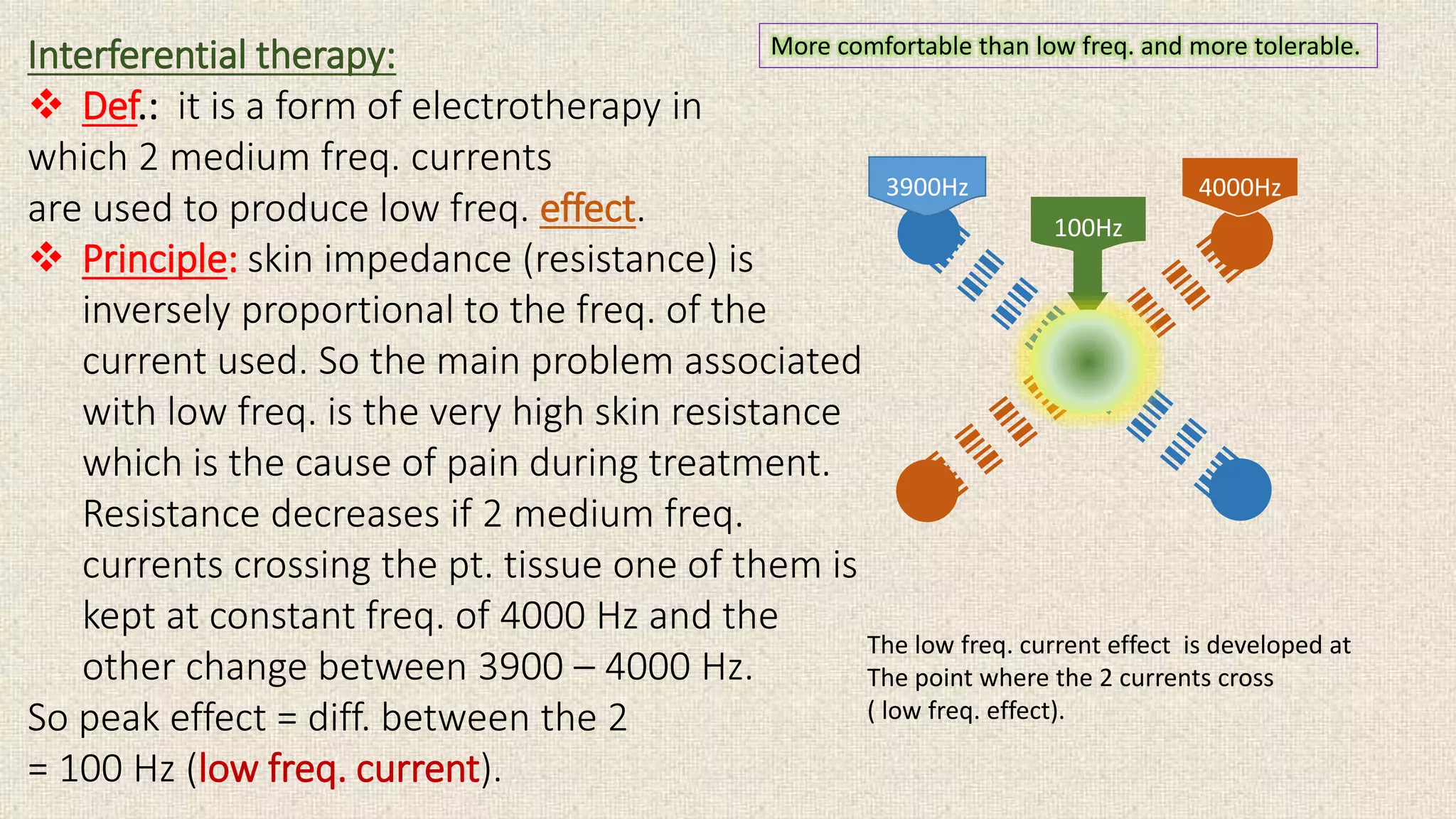
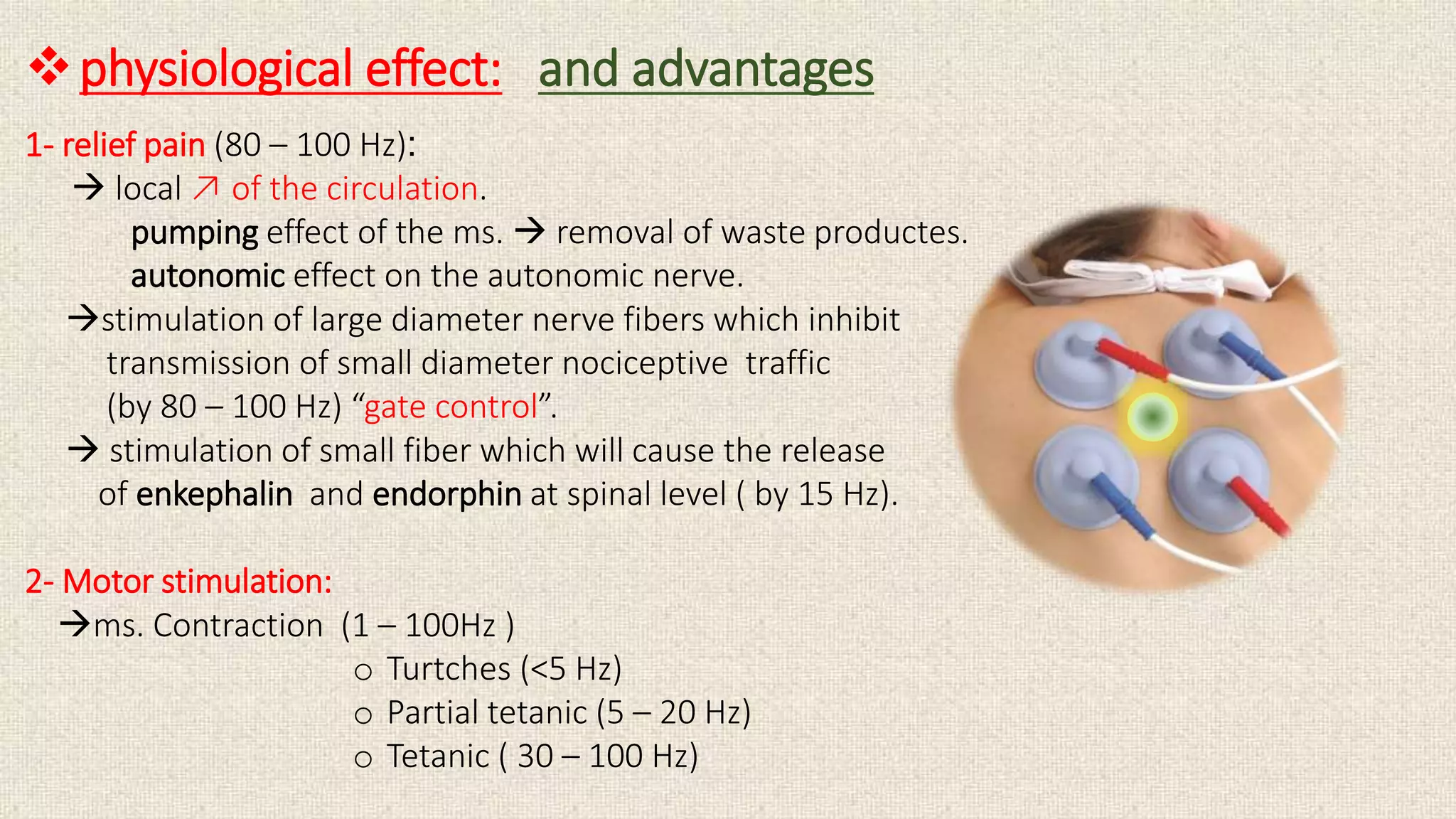
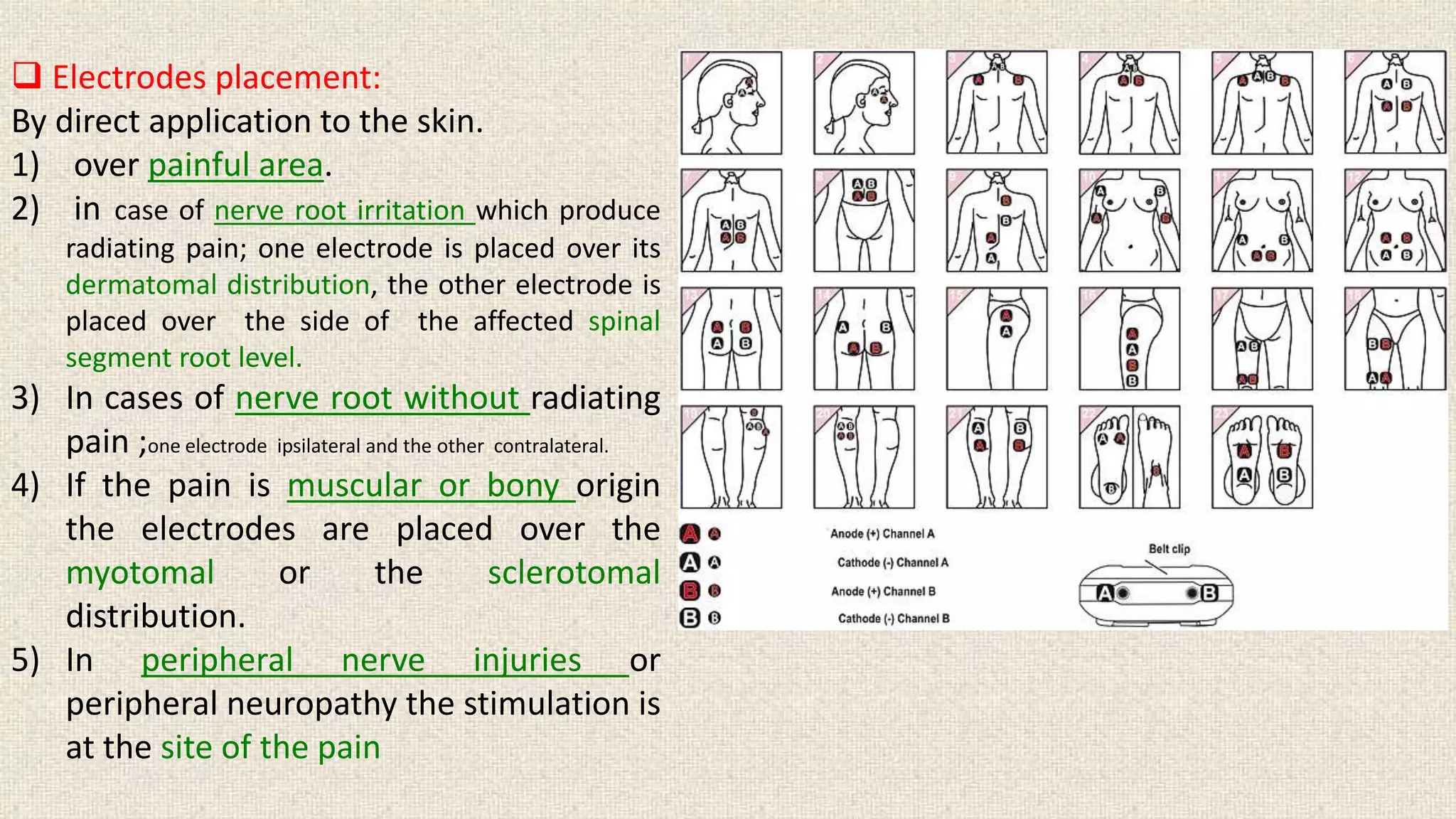
This document discusses various forms of electrotherapy used to treat musculoskeletal disorders. It describes galvanic current, diadynamic current, interferential therapy, and TENS. Galvanic current directly stimulates muscle without activating nerves. Diadynamic current comes in various forms that can stimulate muscles or affect the autonomic nervous system. Interferential therapy uses two medium frequency currents to produce a low frequency effect for pain relief and muscle stimulation. TENS is a form of electrical stimulation that decreases pain by activating sensory nerves via surface electrodes.