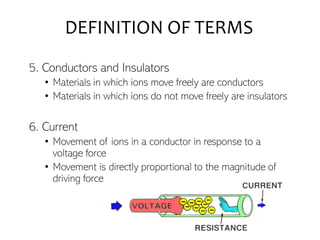
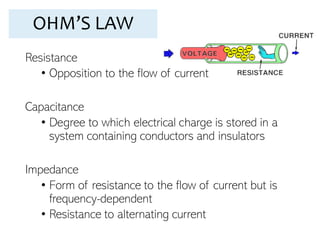
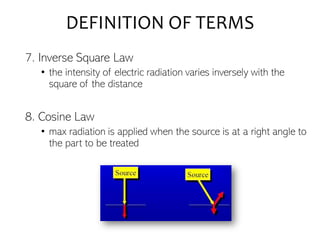
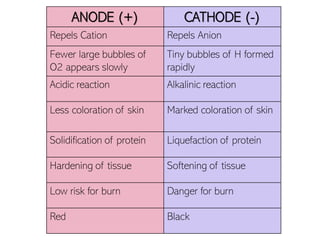
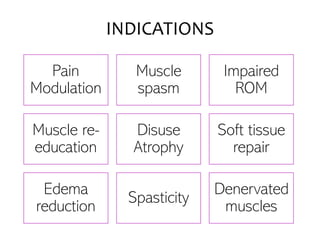
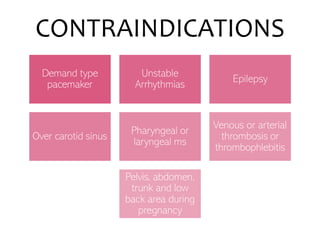
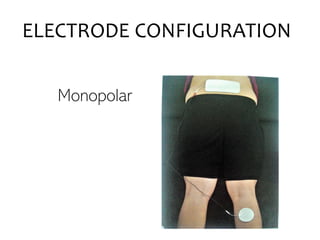
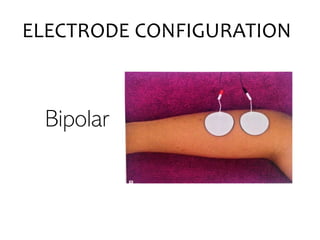
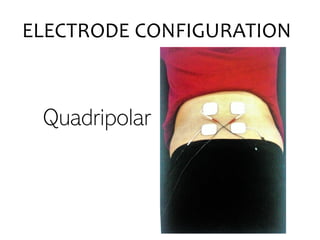
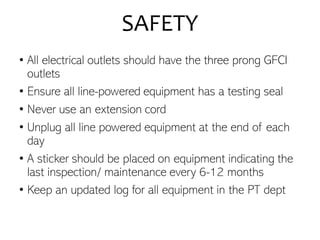
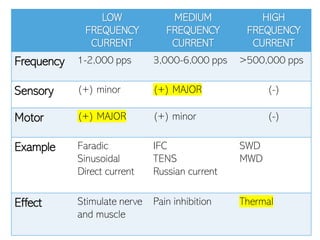
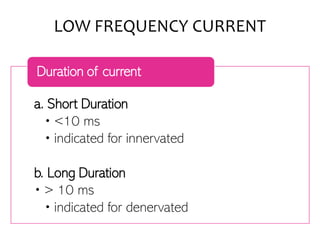
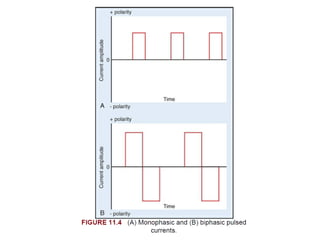
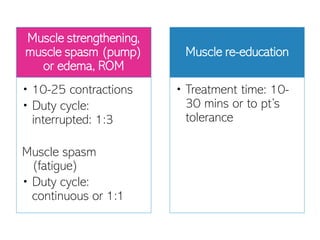
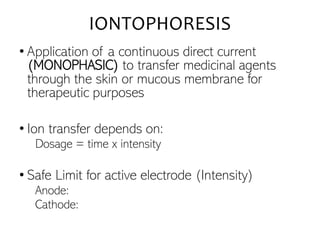
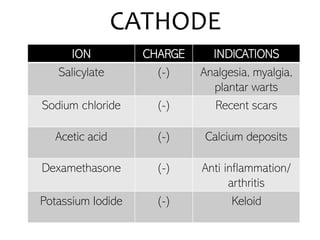
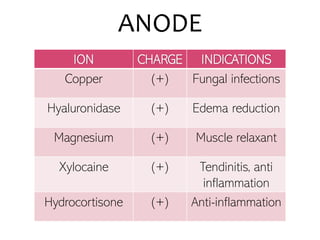
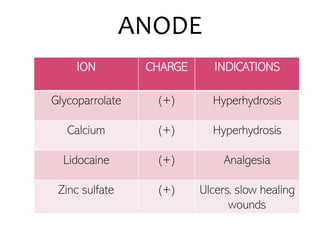
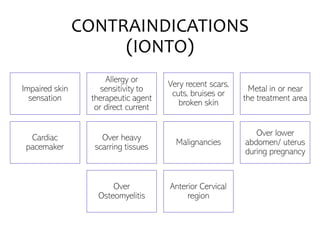
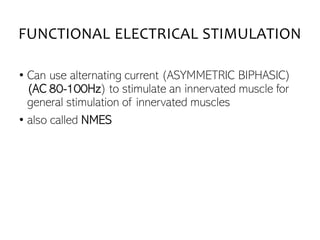
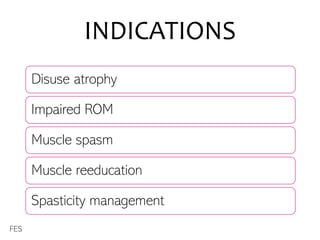
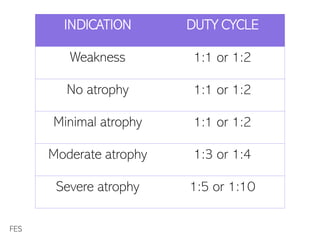
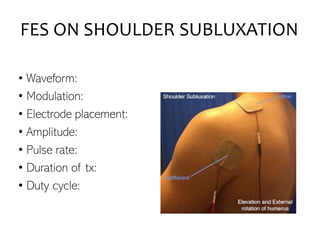
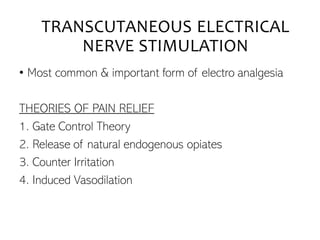
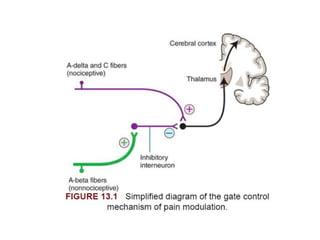
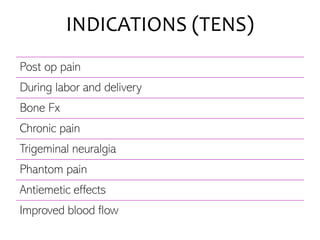
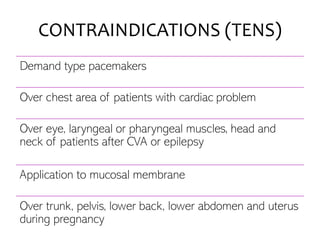
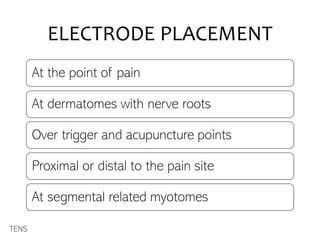
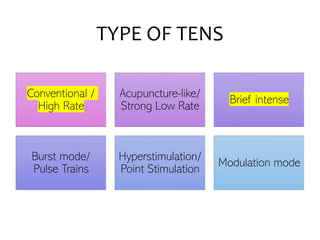
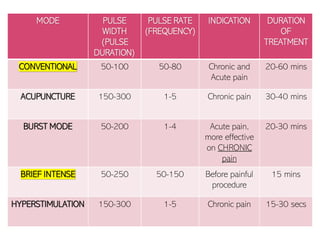
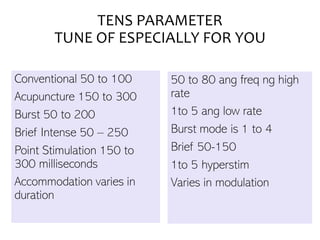
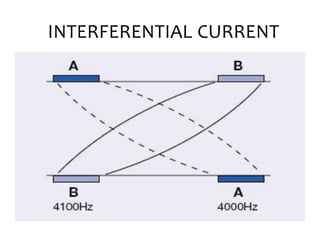
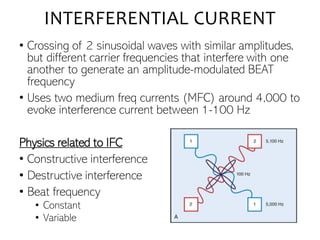
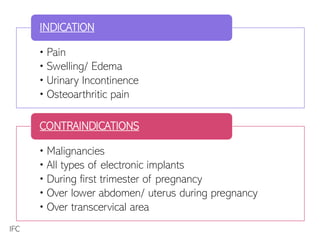
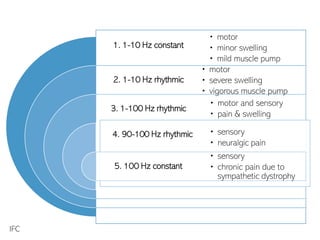
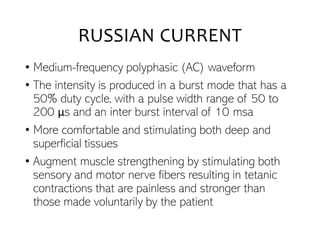
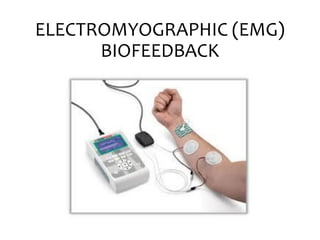
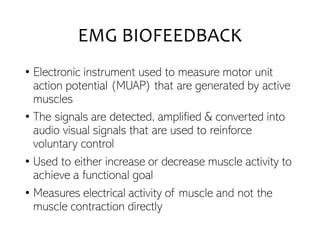
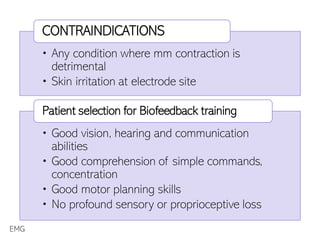
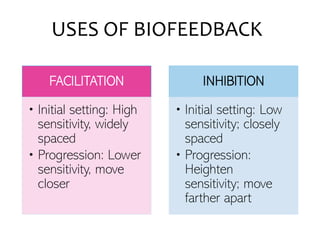
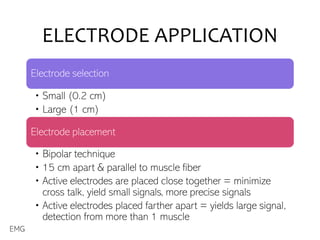
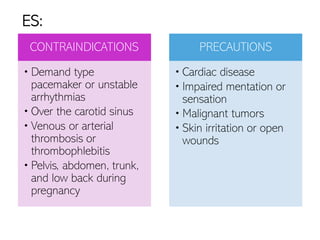
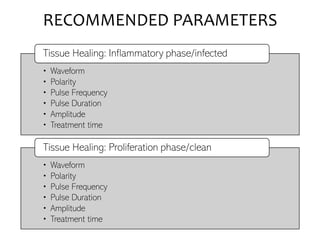
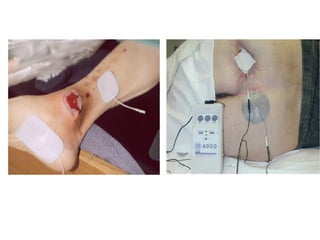
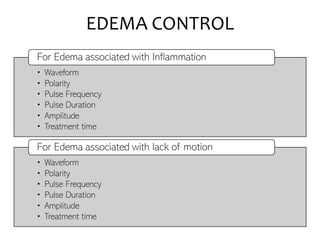
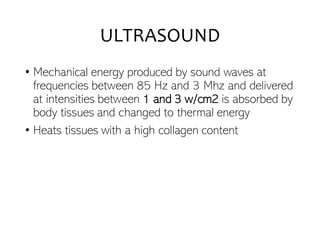
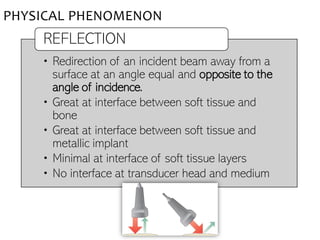
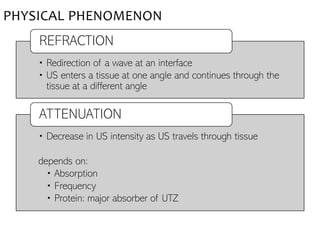
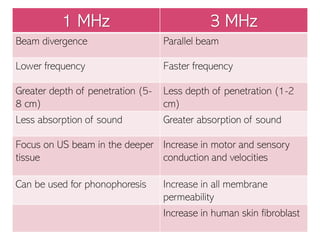
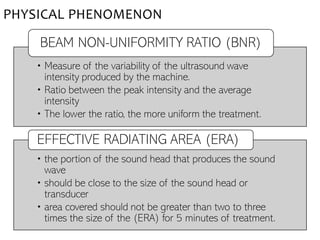
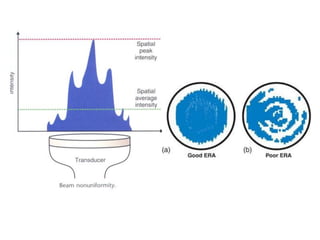
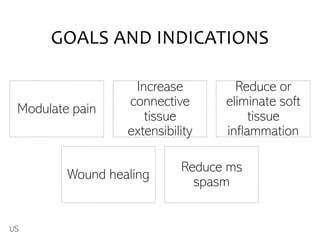
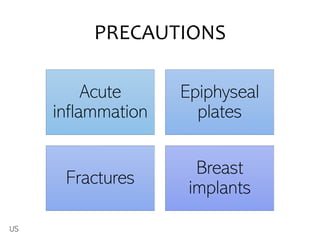
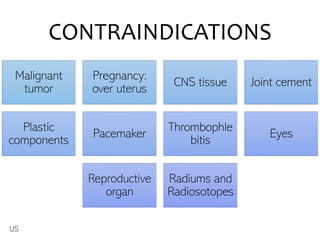
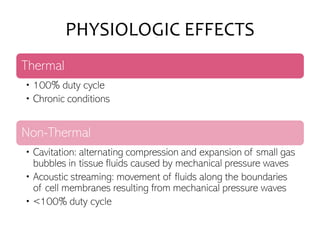
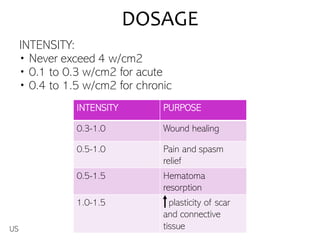
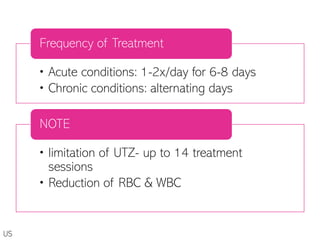
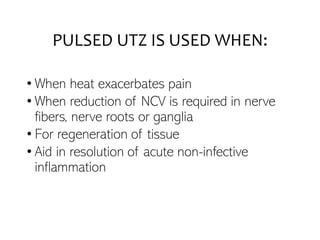
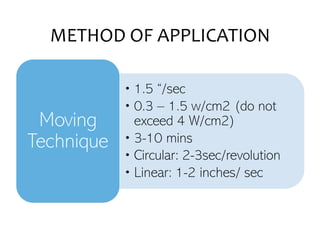
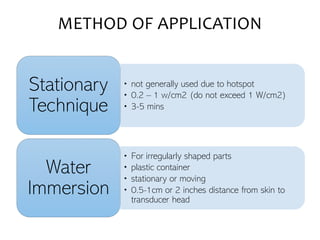
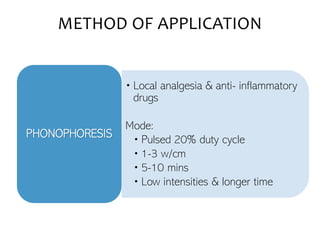
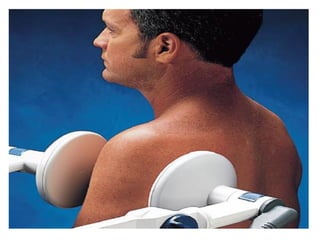
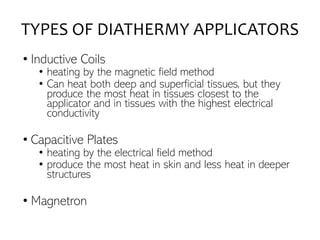
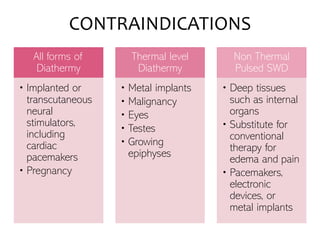
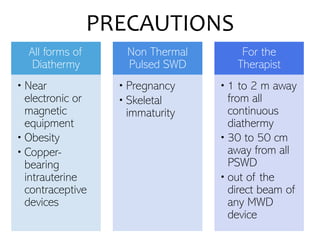
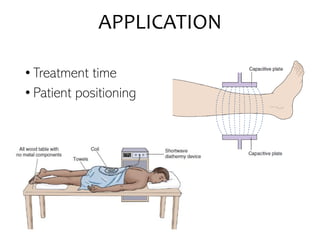
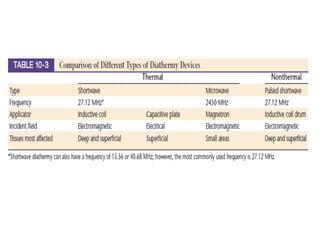
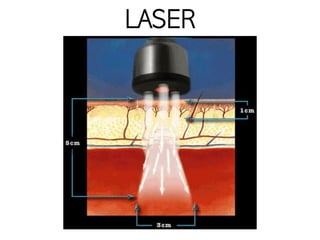
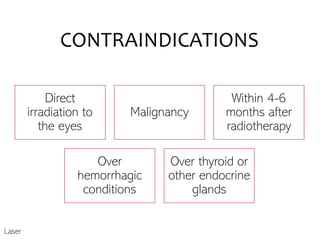
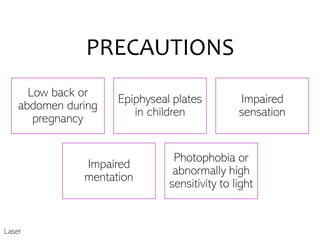
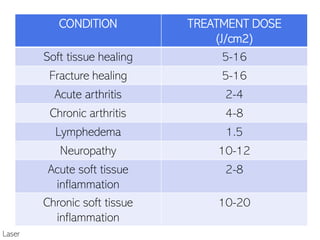
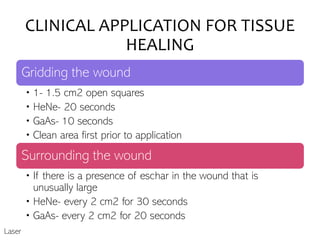
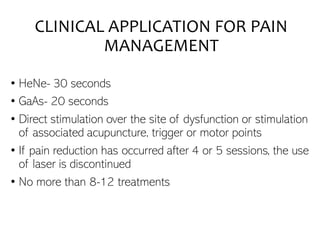
The document provides a comprehensive overview of electrotherapy techniques, including definitions of essential terms, principles of electrical charge, and various modalities like ultrasound, diathermy, and laser treatments. It covers treatment parameters, indications, contraindications, and detailed guidelines for electrode configurations and safety precautions. Additionally, it includes information on biofeedback and the physiological effects of modalities aimed at pain relief and tissue healing.