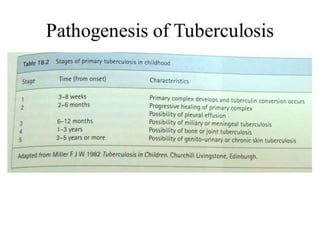
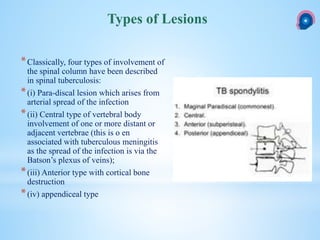
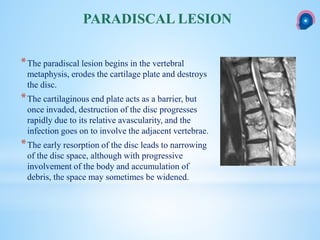
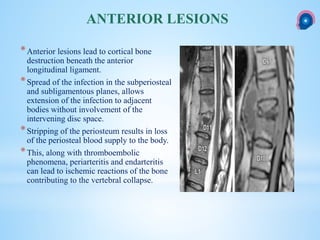
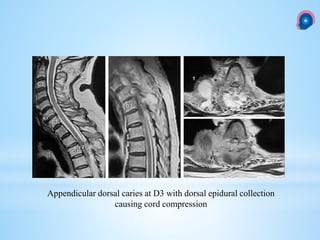
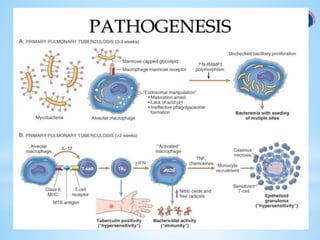
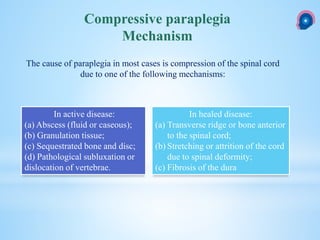
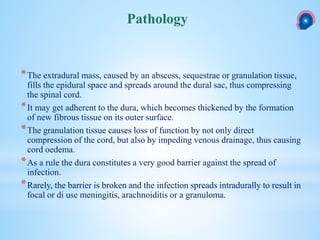
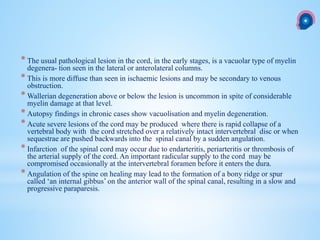
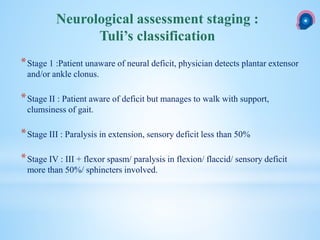
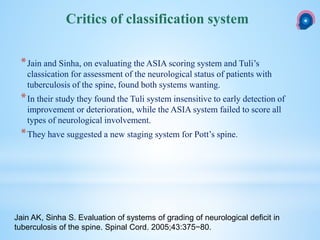
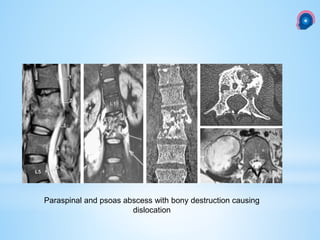
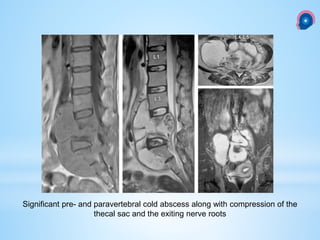
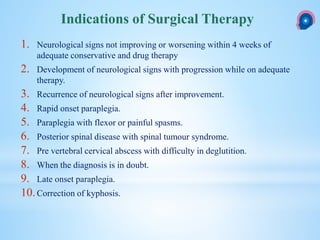
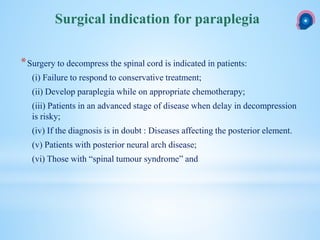
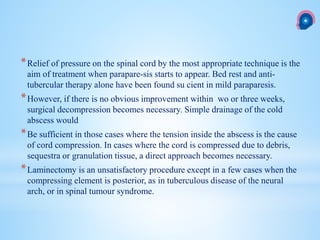
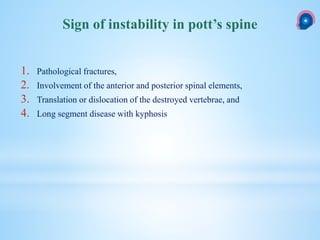
This document provides information on spinal tuberculosis, including its history, types of lesions, clinical presentation, imaging findings, treatment, and indications for surgery. It discusses how spinal tuberculosis is usually secondary to a primary infection elsewhere in the body that spreads hematogenously to the spine. The most common type of spinal lesion is a paradiscal lesion that begins in the vertebral body. Clinical presentation varies from asymptomatic to paraplegia. Imaging like CT and MRI are useful to identify bone destruction and abscesses. Treatment involves anti-tuberculosis medications for 18 months along with rest. Surgery is indicated for neurological deterioration, advanced disease, or diagnostic uncertainty.