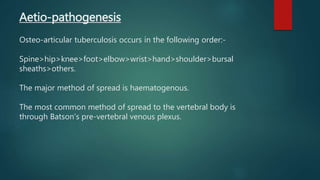
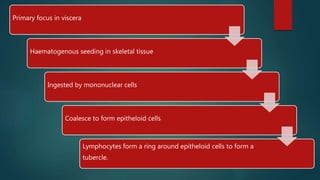
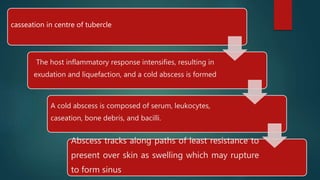
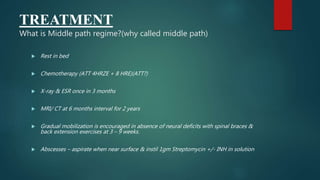
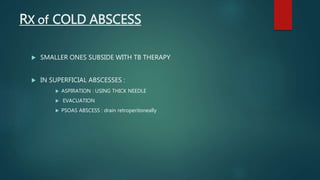
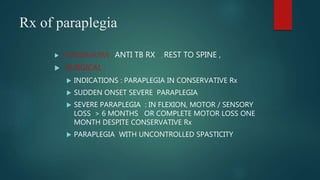
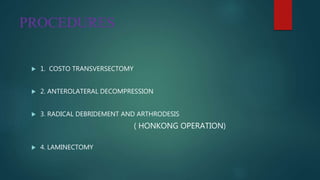
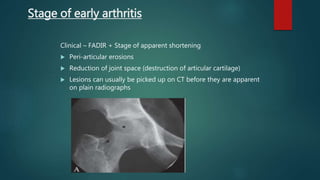
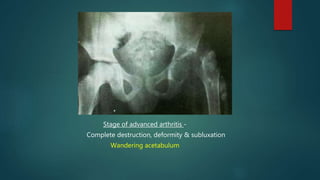
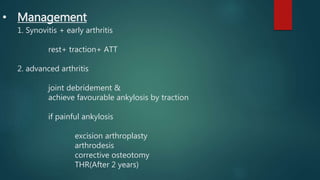
Osteoarticular tuberculosis is a common disease globally and in India, with involvement of bones and joints in around 30% of tuberculosis cases. It occurs most commonly in the spine, hip, knee, and other joints. It spreads hematogenously from a primary pulmonary or other visceral lesion. Spinal involvement often leads to deformities like gibbus formation or neurological complications like paraplegia. Treatment involves anti-tubercular medications like ATT along with rest and surgery if needed to drain abscesses or decompress nerves. Hip involvement can progress through stages of synovitis, arthritis, and advanced destruction requiring treatments like joint debridement, arthrodesis, or excision arthroplasty.