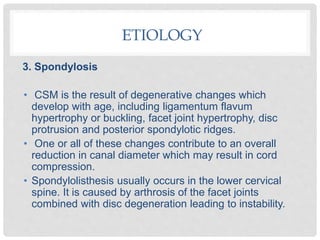
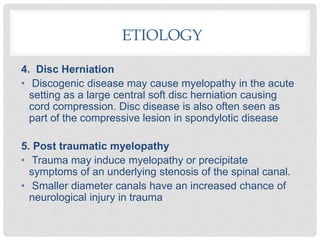
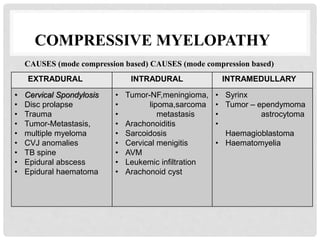
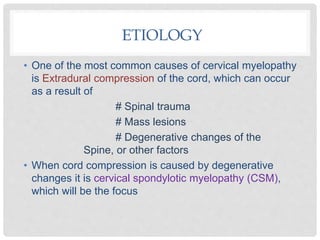
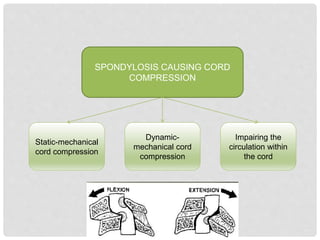
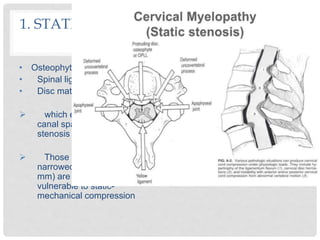
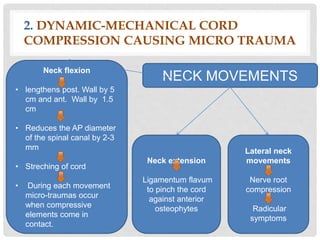
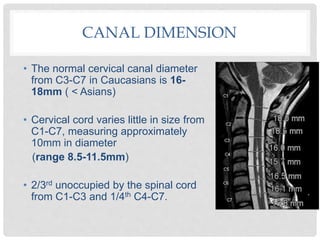
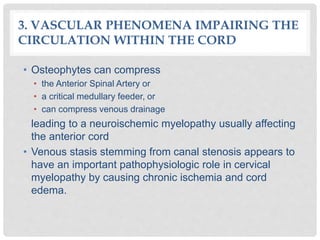
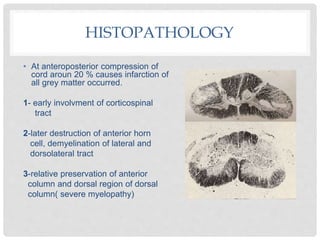
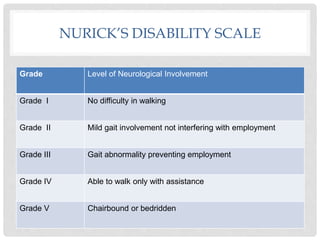
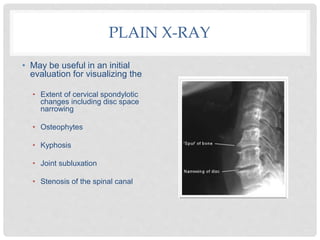
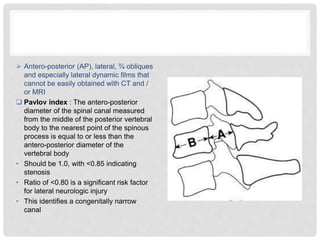
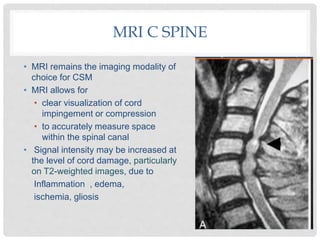
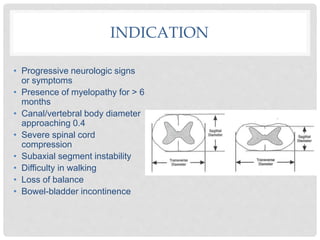
Cervical myelopathy is caused by compression of the cervical spinal cord, most commonly from cervical spondylosis. Cervical spondylosis involves degenerative changes to the spine that decrease space for the spinal cord. This can lead to static or dynamic compression of the cord, impairing circulation. Patients experience symptoms like neck pain, weakness, spasticity and sensory changes. Diagnosis involves assessing severity using scales and investigating spinal changes through imaging like CT which shows stenosis and compression more clearly than x-rays.