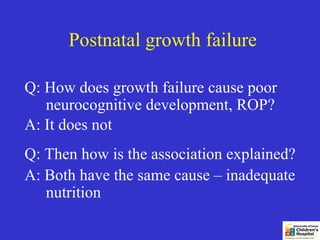
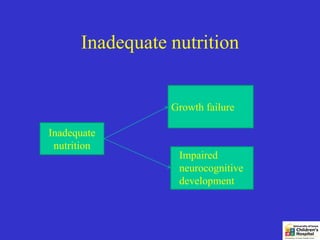
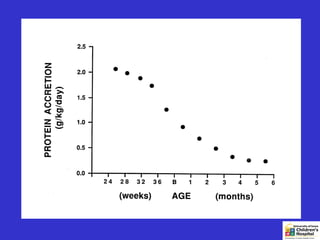
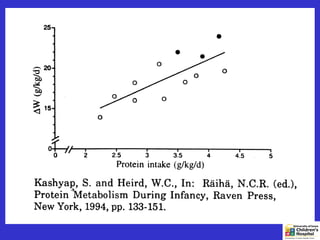
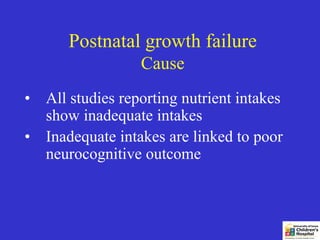
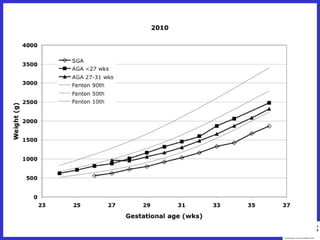
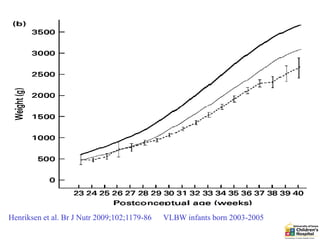
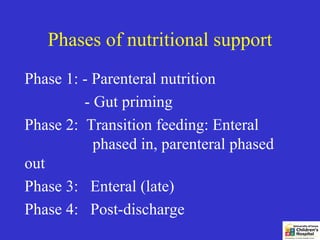
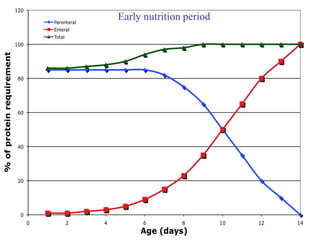
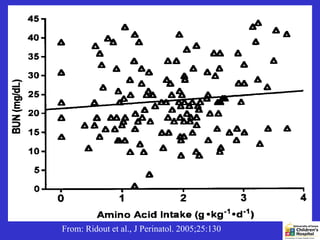
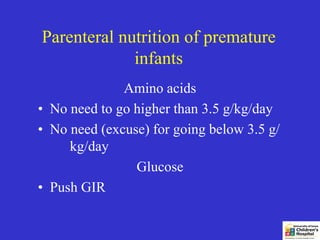
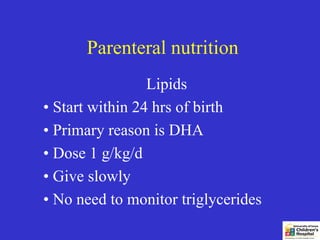
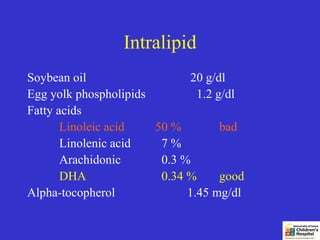
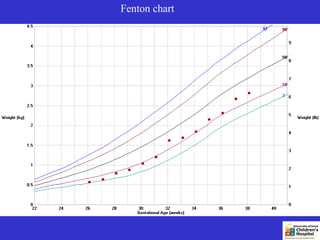
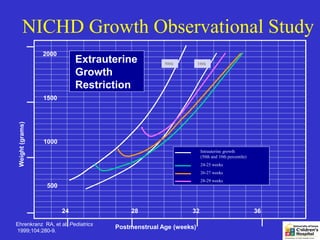
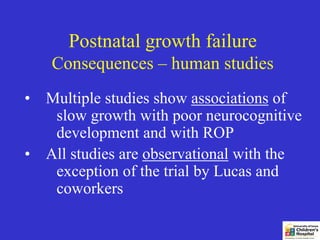
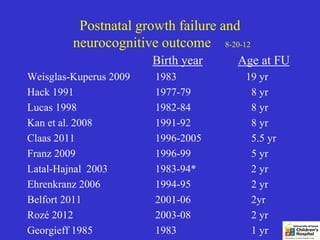
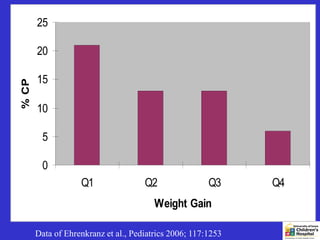
The document discusses postnatal growth failure in premature infants, emphasizing its consequences on neurocognitive development and the importance of nutritional support. It outlines the phases of nutritional support, including parenteral and enteral nutrition strategies, to prevent growth failure. Additionally, it highlights the correlation between inadequate nutrition and poor developmental outcomes.
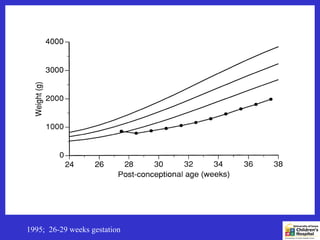

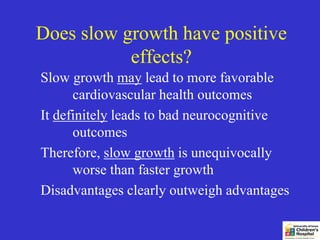
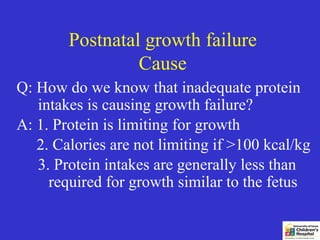
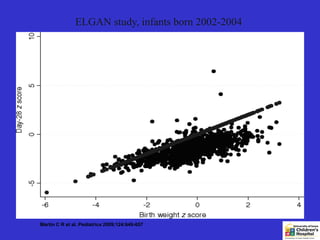
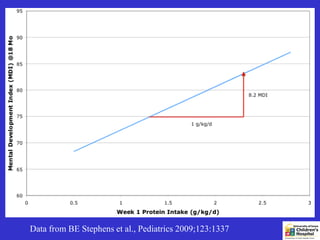
![Growth 1 Week to Term and
18-month Bayley scores
Belfort et al., Pediatrics 2011;128:e899-e906
(Data from Australian DINO study [high-dose DHA] conducted by
Makrides & Gibson 2001-2005; infants <33 wks)
Points per 1 z-score increment
MDI PDI
All infants 2.4 (0.8 - 3.9) 2.7 ( 1.2 - 4.2)
<1250 g 4.7 (2.1 - 7.4) 5.9 ( 3.2 - 8.6)
>1250 g 1.0 (-0.8 - 2.8) 0.8 (-0.9 - 2.5)
AGA 1.6 (0.0 - 3.3) 1.9 (0.3 - 3.5)
SGA 11.7 (4.5 - 18.8) 11.2 (1.8 - 20.7)](https://image.slidesharecdn.com/201zieglereng-130317090120-phpapp01/85/Postnatal-growth-failure-and-its-prevention-16-320.jpg)