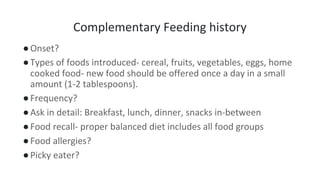
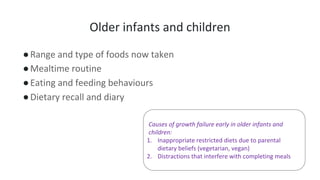
Here are the key points to discuss regarding the importance of feeding history in assessing failure to thrive:
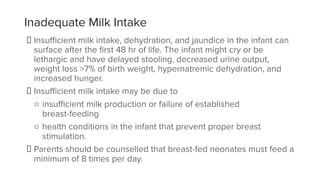
- Feeding history provides important information about quantity and quality of milk intake, which is crucial to evaluate nutritional status and growth. Insufficient intake can lead to failure to thrive.
- It identifies issues like improper formula preparation which can cause electrolyte imbalances and affect growth. Common issues are over-dilution reducing nutrients or concentration causing dehydration.
- For breastfed infants, history on breastfeeding patterns reveals issues like poor latch or milk production which impact nutrition. It evaluates if exclusive or mixed feeding and assesses breastmilk intake.
- Changes in feeding amounts and methods over time help identify when growth faltering