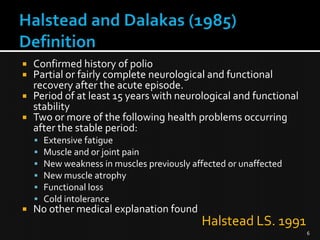
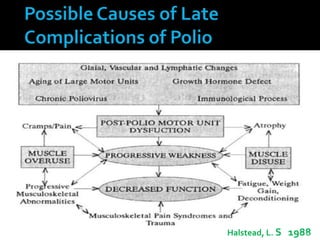
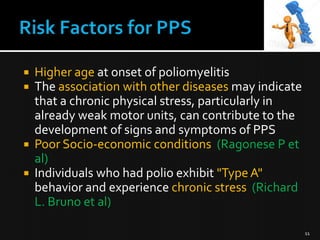
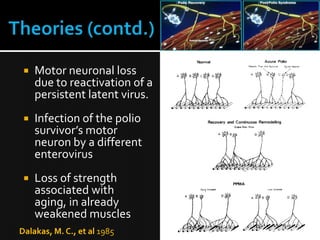
This document discusses post-polio syndrome (PPS), including its definition, epidemiology, causes, clinical features, management, and prognosis. PPS is characterized by new symptoms that emerge decades after an initial bout of paralytic polio, including fatigue, muscle weakness, pain, and loss of function. While the exact pathophysiology is unknown, it is thought to involve the overuse and aging of motor neurons damaged during the initial polio infection. Management focuses on rehabilitation, medication for symptoms, lifestyle modifications, and assistive devices. Prognosis is generally good with treatment, though severe pulmonary or swallowing involvement can be life-threatening in rare cases.

![
Virus [ Burnhilde, Lansing & Leon]
Contaminated water / food
Affinity for motor (muscle) nerves
Kills / Injures motor nerves
Results in weakness / paralysis
3](https://image.slidesharecdn.com/postpoliosyndrome-131114125433-phpapp01/85/Occupational-Therapy-management-for-Post-polio-syndrome-3-320.jpg)