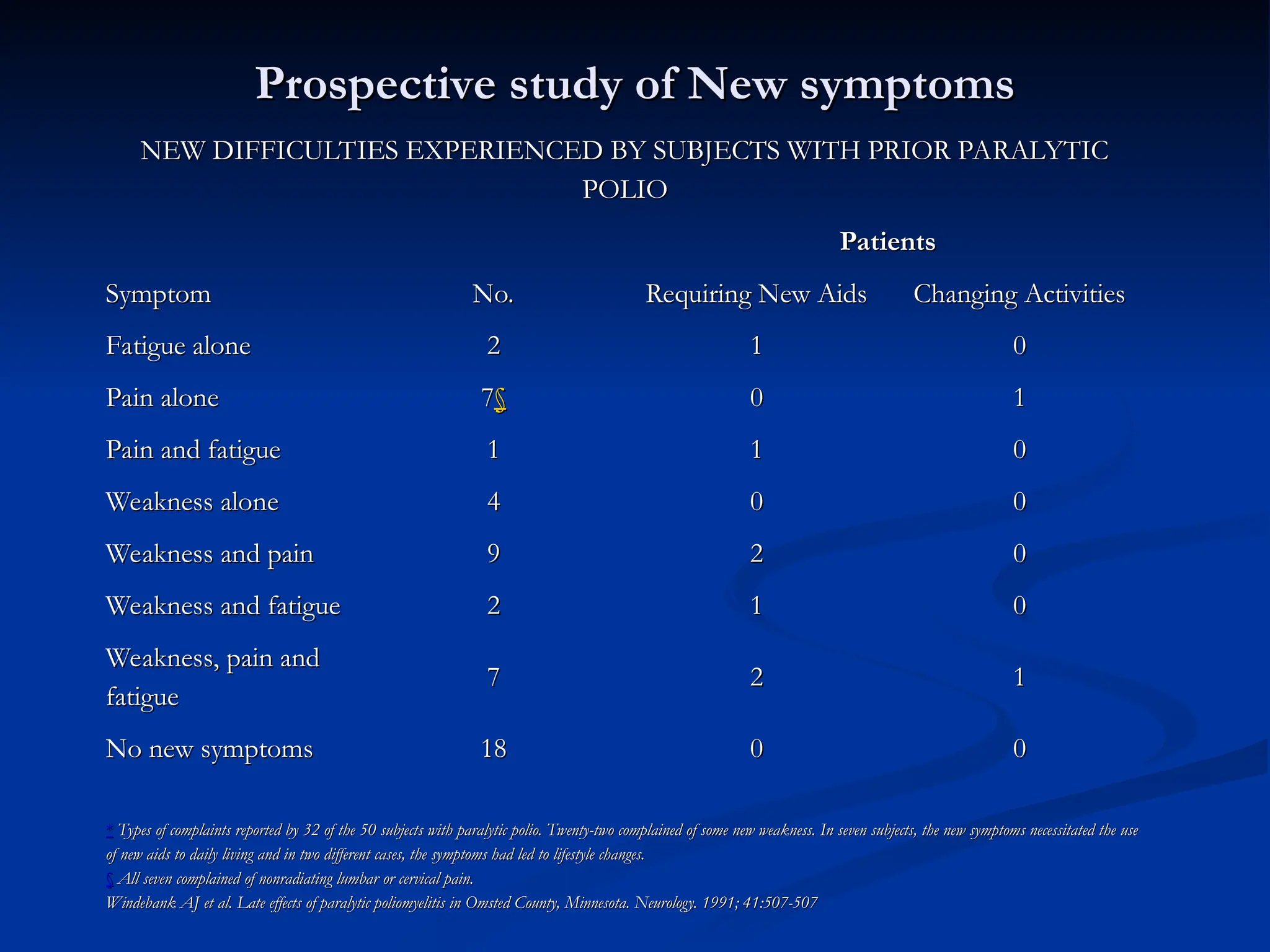
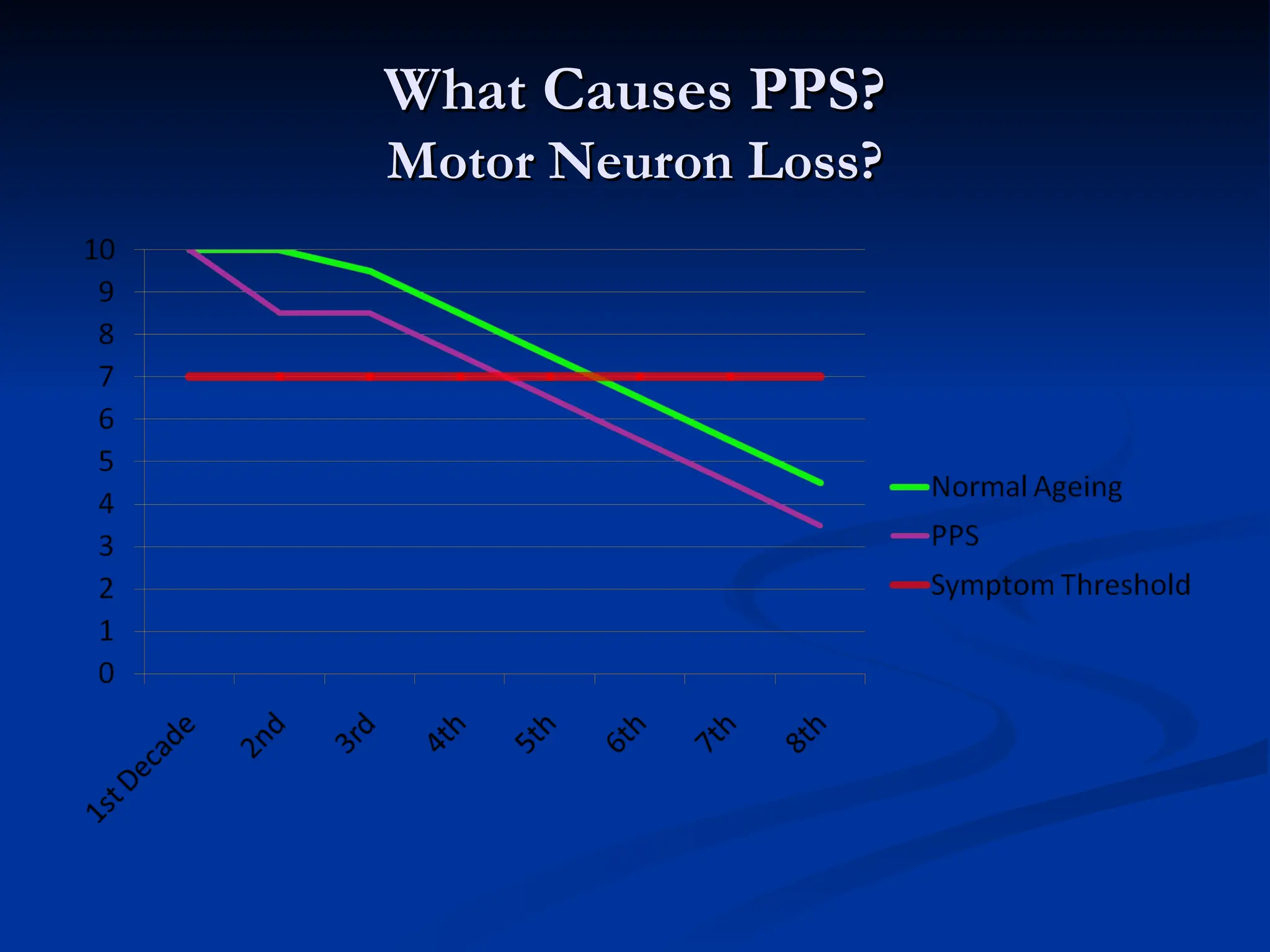
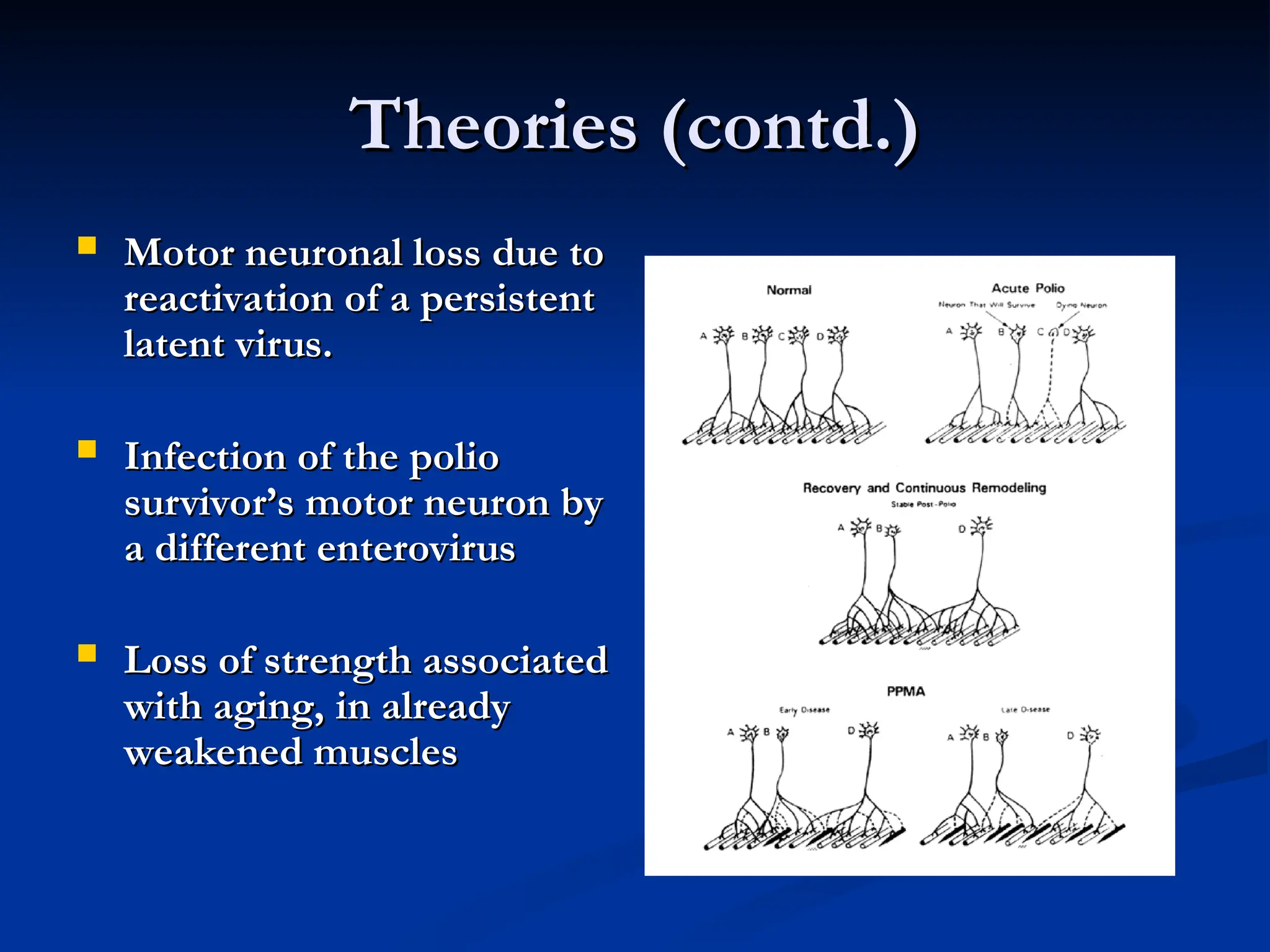
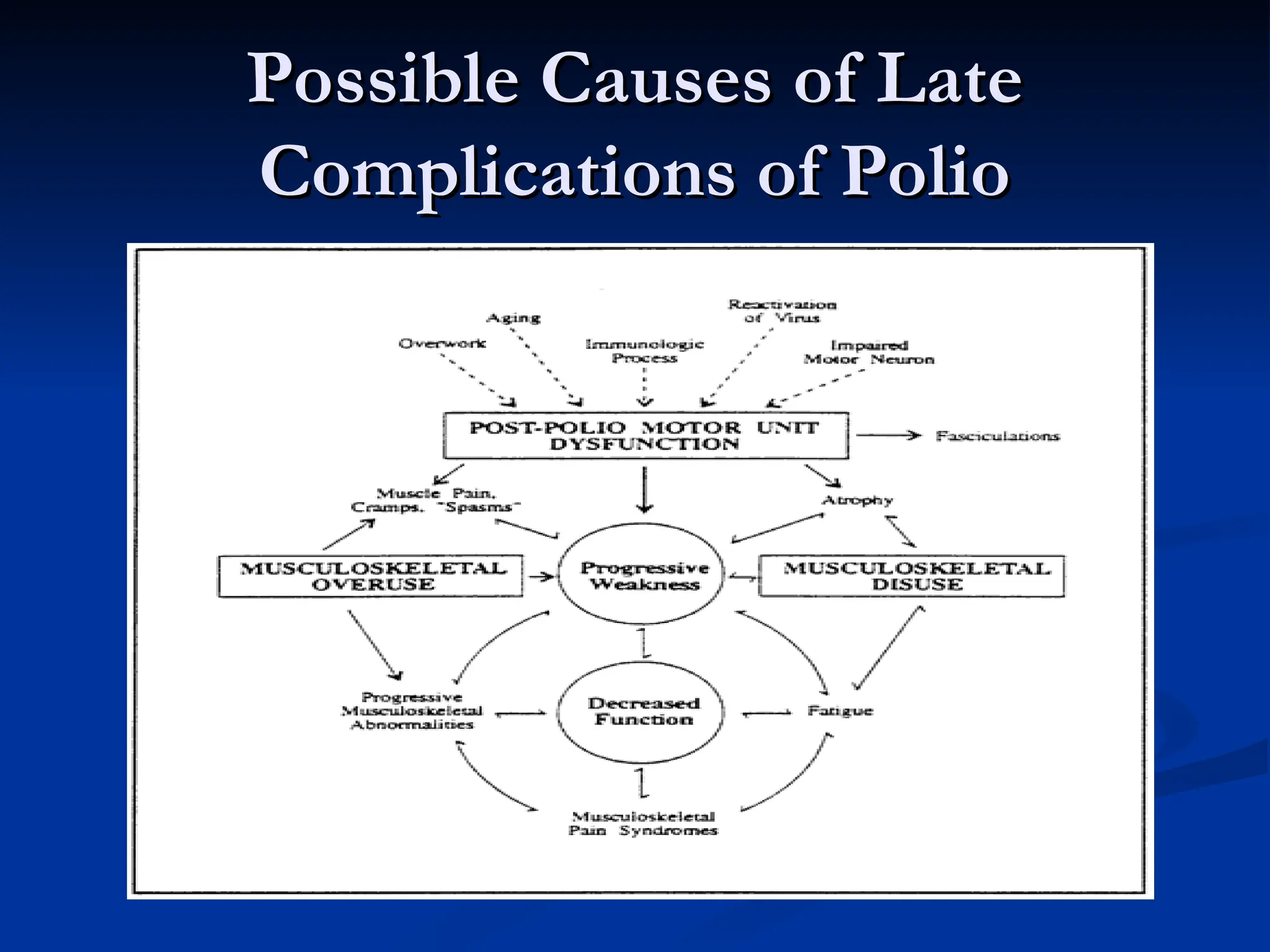
The document discusses the diagnosis and management of post-polio syndrome (PPS), including its historical context, common symptoms, and epidemiology. Key features include fatigue, muscle pain, and weakness, while various theories about the causes of PPS are presented. It highlights the importance of managing co-morbidities and outlines strategies for rehabilitation and maintaining quality of life for affected individuals.