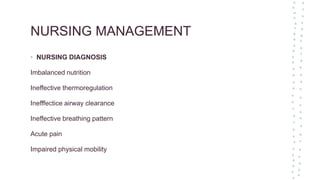
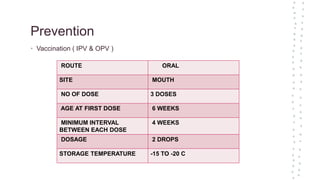
This document appears to be notes from a presentation on Poliomyelitis (Polio). It covers topics such as the causative agent (Poliovirus), modes of transmission (fecal-oral route), risk factors (age, lack of immunization), clinical features (asymptomatic, abortive polio, paralytic forms), diagnosis (cultures, spinal fluid exam), treatment (supportive care, physical therapy), prevention (vaccination schedules), and nursing management considerations. The presentation provides an overview of Polio from its introduction and pathogenesis through clinical presentation, diagnosis, treatment and prevention.