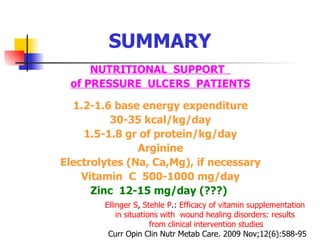
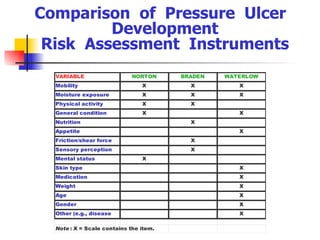
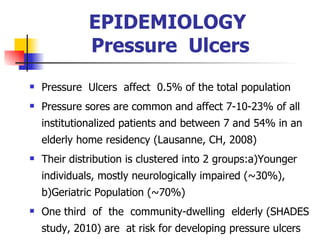
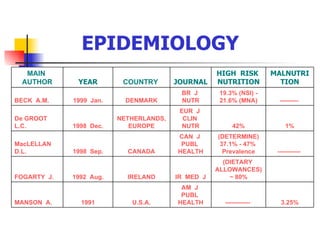
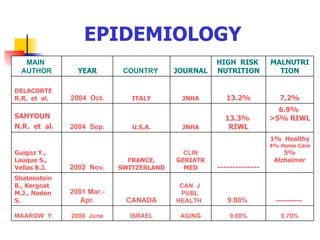
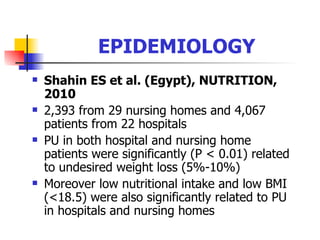
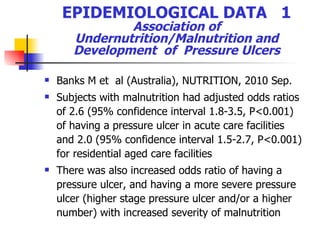
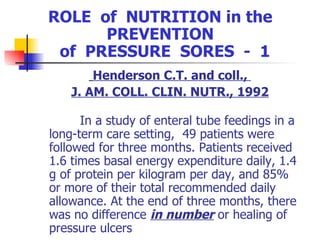
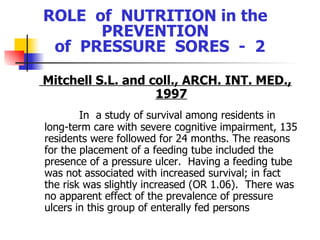
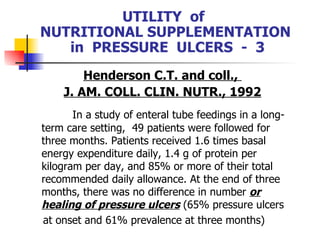
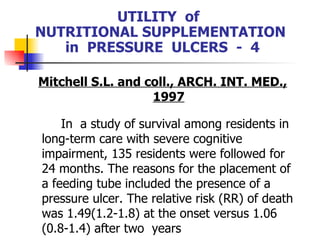
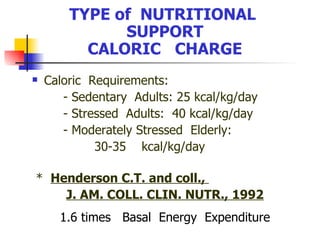
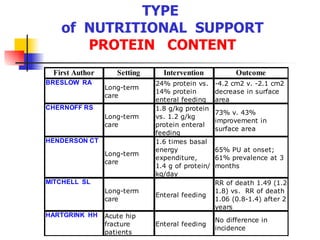
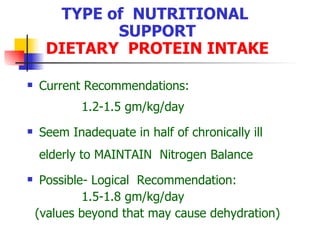
This document discusses the relationship between nutritional status and pressure ulcers. It provides epidemiological data showing that malnutrition is associated with increased risk of developing pressure ulcers. Experimental studies in animals also demonstrate impaired wound healing in malnourished subjects. However, clinical studies on the effect of nutritional supplementation on pressure ulcer prevention and treatment have shown mixed results, with some finding no effect of supplementation on ulcer outcomes. Overall, while malnutrition and pressure ulcers often coexist, the relationship is complex and a causal link has not been firmly established.
![TYPE of NUTRITIONAL SUPPORT SPECIFIC NUTRIENTS: AMINOACIDS - 1 Arginine [8.5gr, 17gr/day] does not enhance Lymphocyte Proliferation or Interleukin Production, Langkamp-Henken B. and coll., JPEN, 2000](https://image.slidesharecdn.com/spatharakis-110606052012-phpapp01/85/Spatharakis-36-320.jpg)
![TYPE of NUTRITIONAL SUPPORT SPECIFIC NUTRIENTS: VITAMIN C - 3 Ter Riet G. et al., J.CLIN.EPIDEMIOL.,1995 The objective of this study was to assess the effects of ascorbic acid supplementation, 500 mg twice daily in the treatment of pressure ulcers of 88 patients in a blinded randomized trial over 12 weeks. A nalysis showed that the wound closure rate was not higher in the intervention group than in the control group (Cox hazard ratio of 0.78 [90% precision interval, 0.44-1.39]). Mean absolute healing rates were 0.21 and 0.27 cm2/week in the intervention and control group, respectively (PI of the adjusted difference: -0.17 to 0.13). Relative healing rates and healing velocities did not show favorable results of ascorbic acid supplementation, either. The improvement was 0.45 and 0.72 points per week in the intervention and control group, respectively](https://image.slidesharecdn.com/spatharakis-110606052012-phpapp01/85/Spatharakis-42-320.jpg)