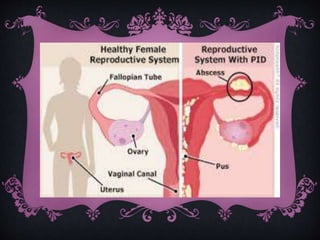
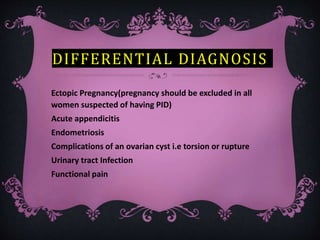
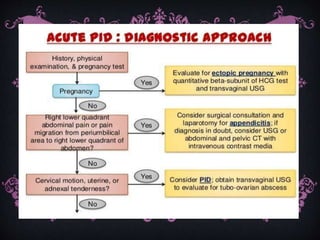
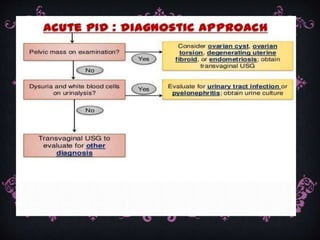
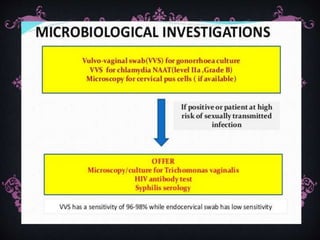
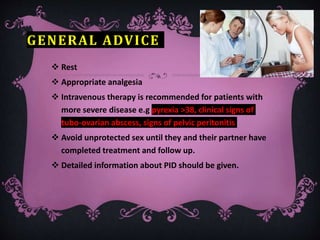
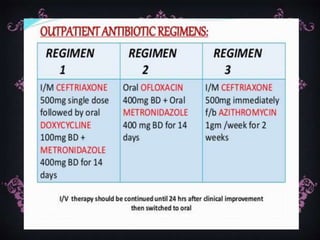
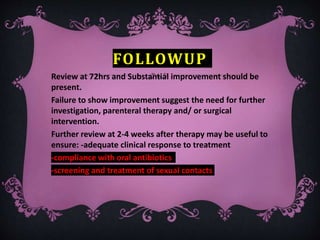
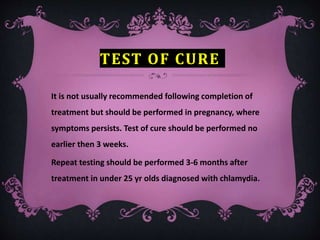
PID is an inflammatory condition of the female upper genital tract caused by bacteria like Neisseria gonorrhoeae and Chlamydia trachomatis. Risk factors include young age, multiple sexual partners, and IUD insertion within 6 weeks. Symptoms include lower abdominal and pelvic pain. Treatment involves broad spectrum antibiotics as soon as possible to prevent long term complications like infertility. Sexual partners also need treatment to prevent reinfection. Follow up is needed to ensure clinical response and partner treatment.