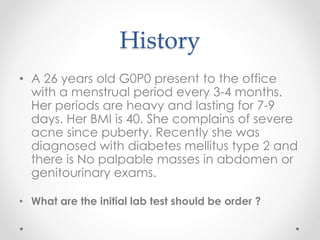
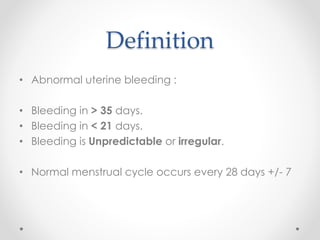
This document discusses abnormal uterine bleeding, including its definition, causes, approach to diagnosis, and management. It defines different types of abnormal bleeding and notes that the most common causes in reproductive-aged women are ovulatory dysfunction and anovulation. The initial workup involves a medical history, physical exam, and basic lab tests. Further testing may include ultrasounds, endometrial biopsies, or hysteroscopies. Treatment depends on the underlying cause but often involves hormonal therapy as first-line treatment or surgical options if medical management fails or is contraindicated.