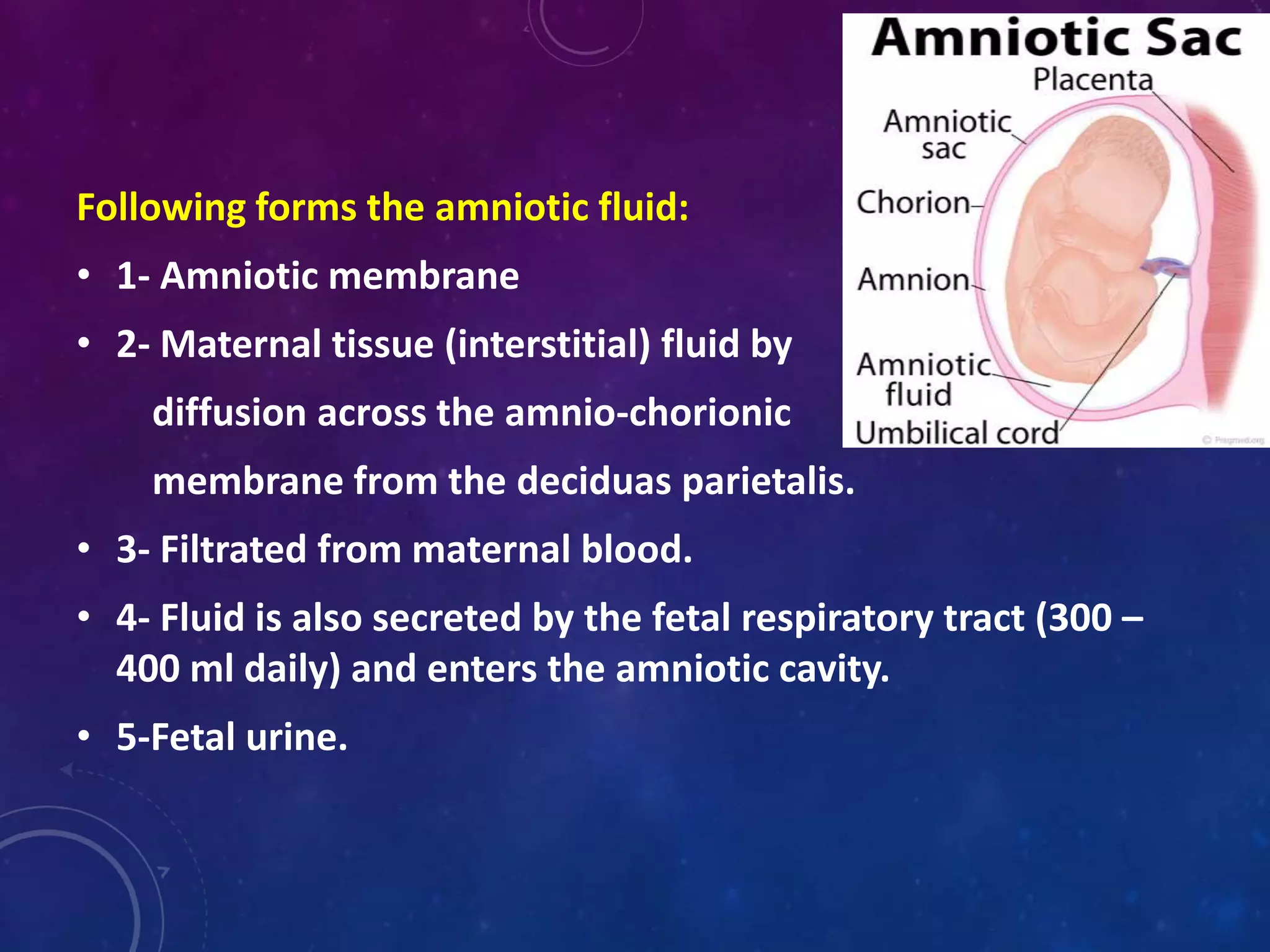
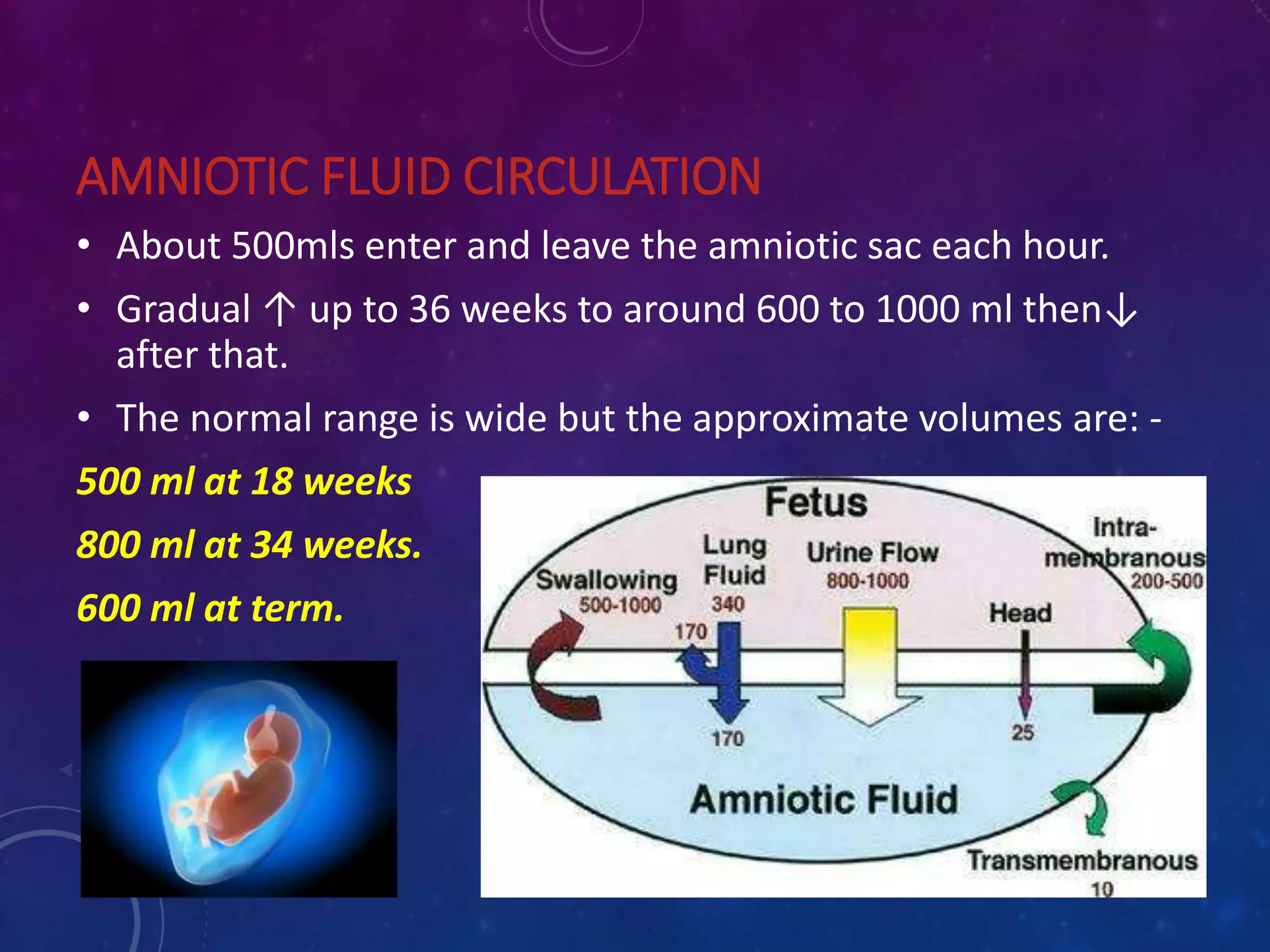
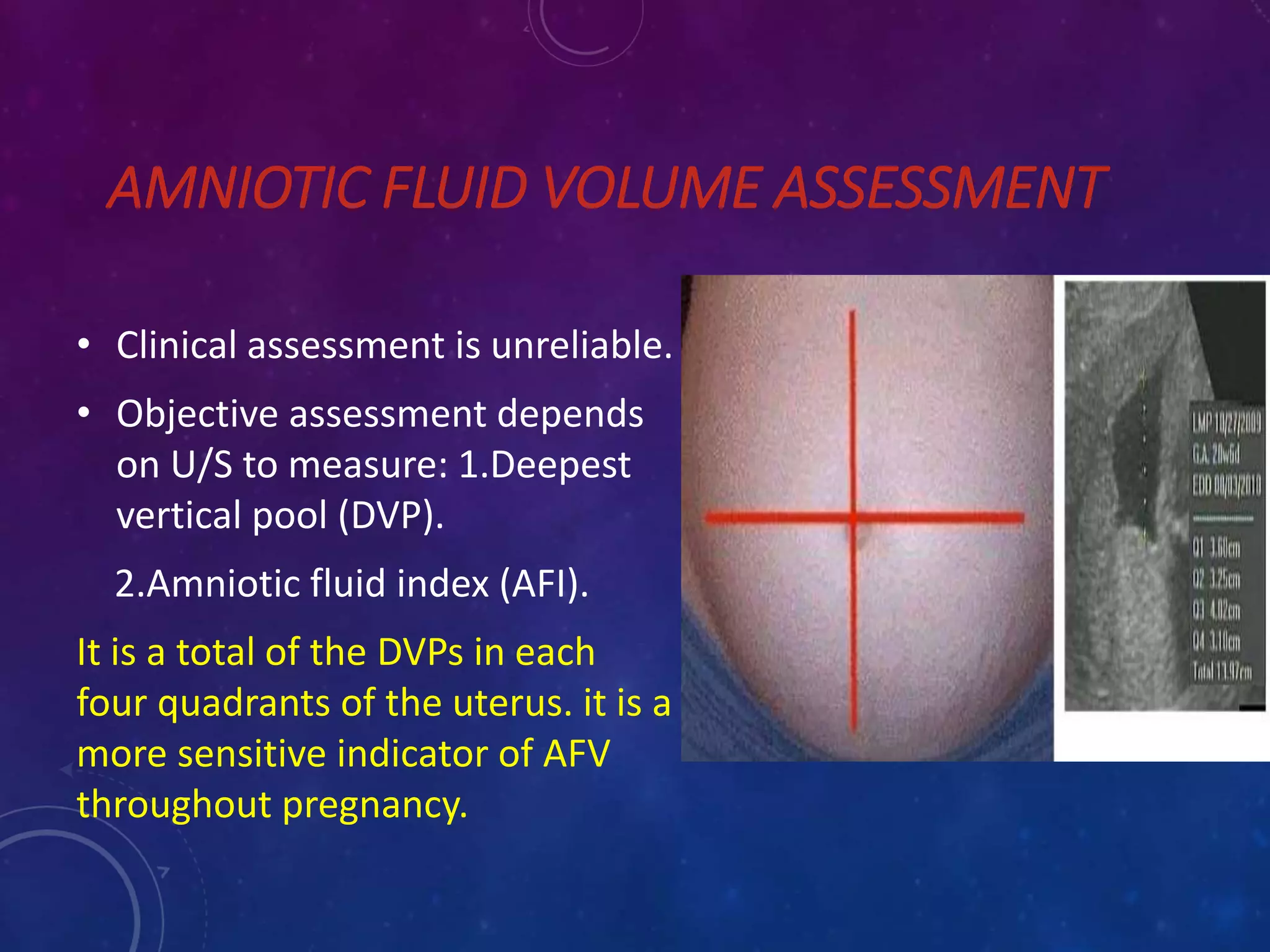
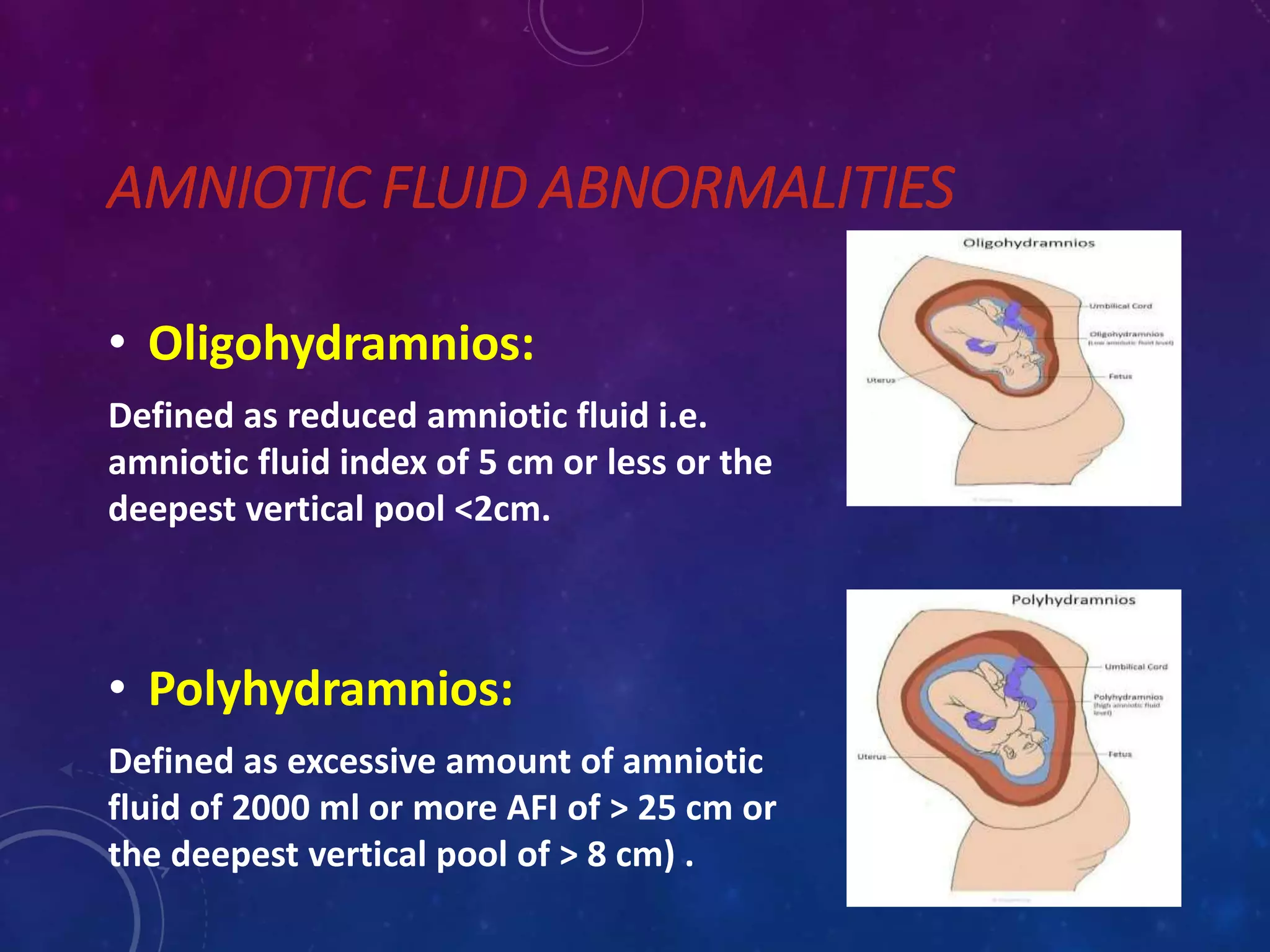
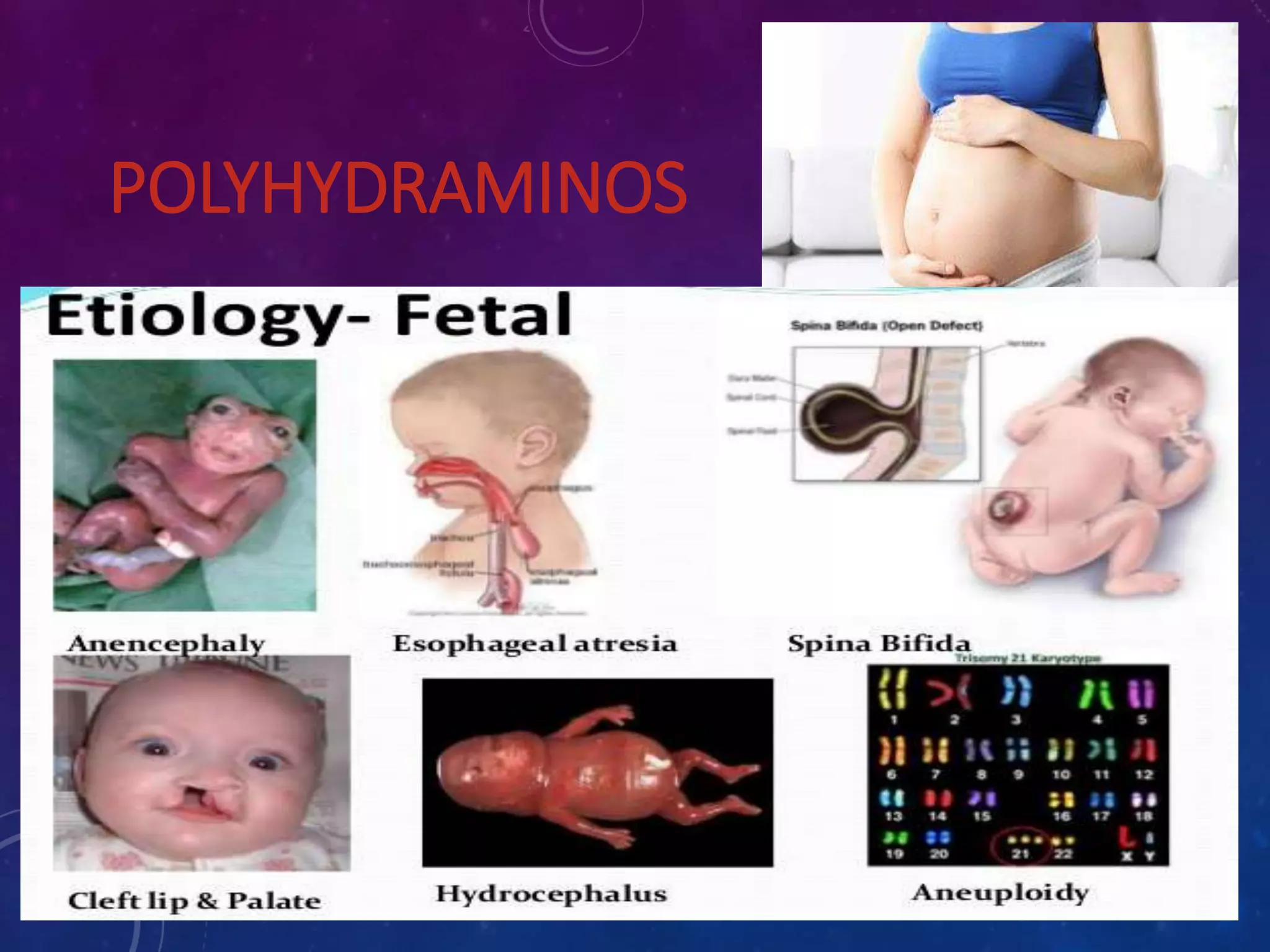
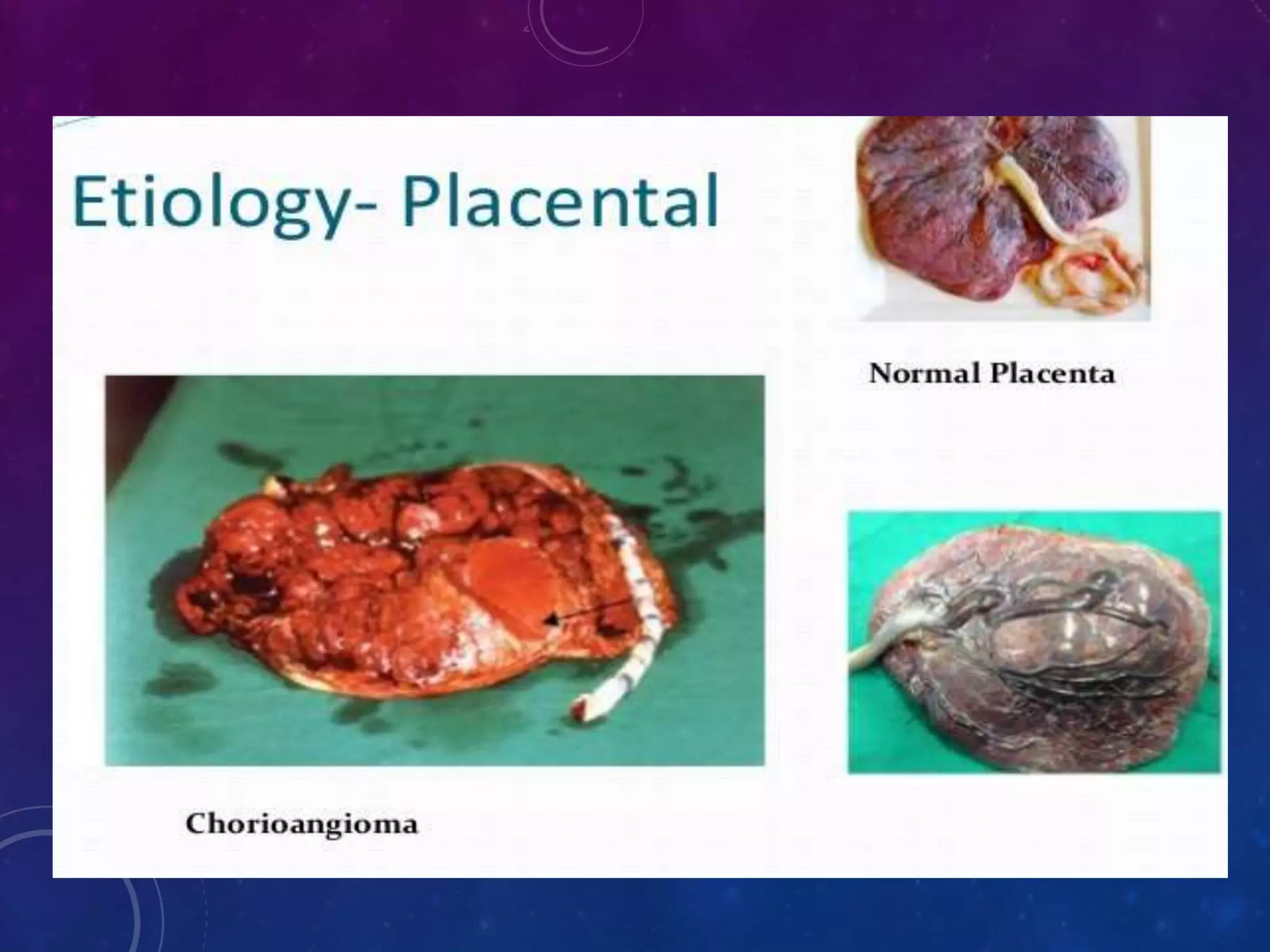
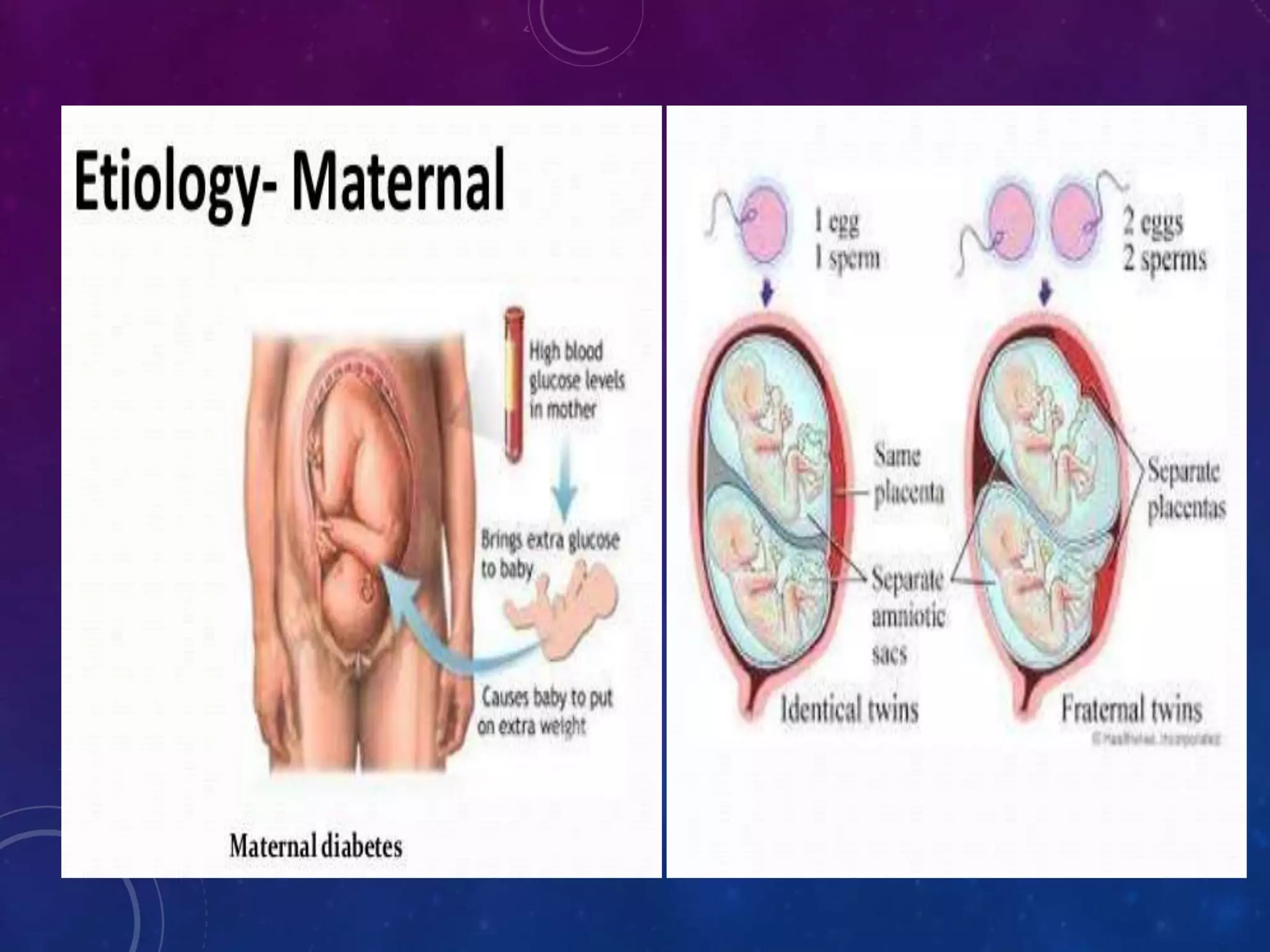
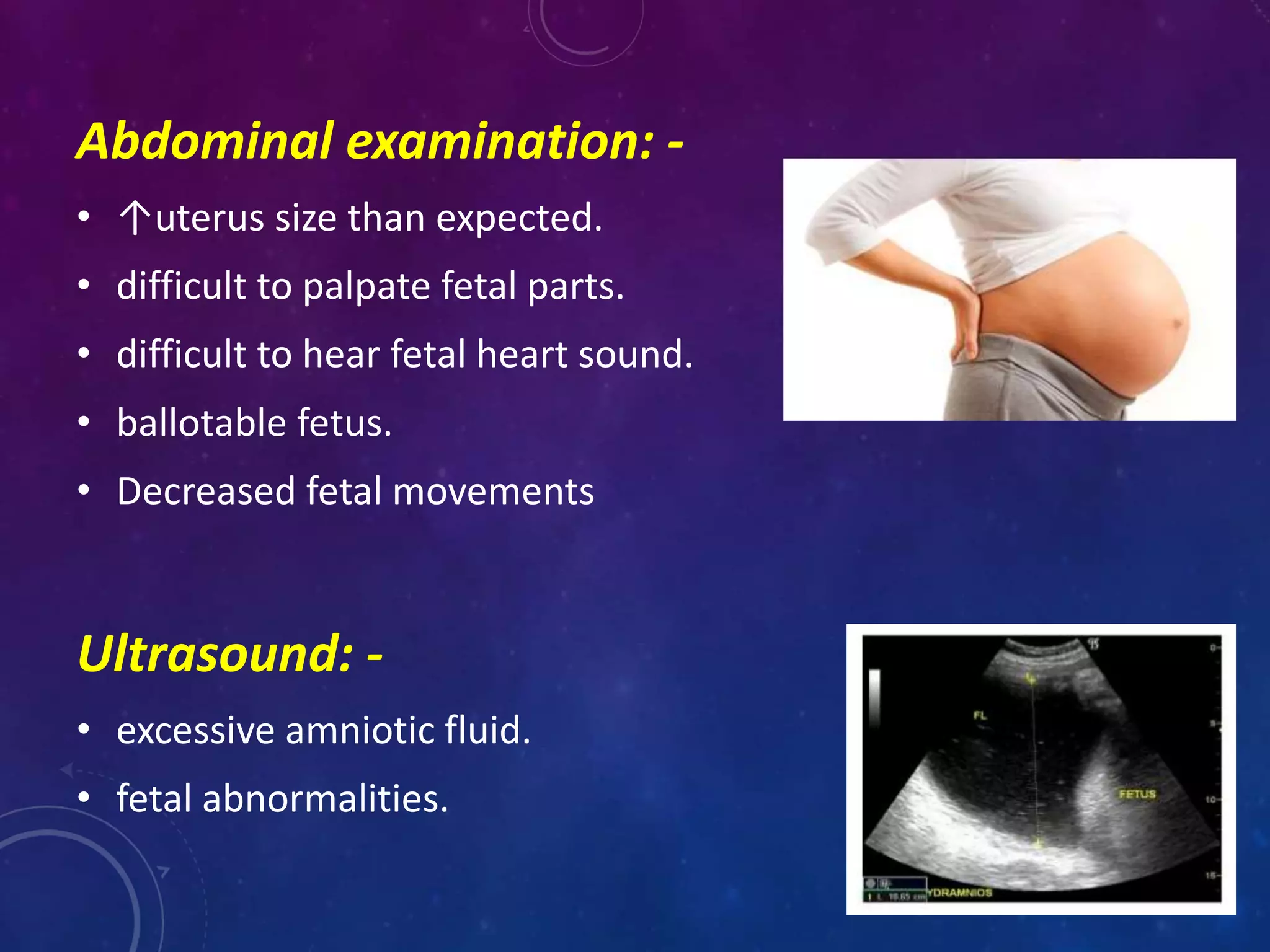
Amniotic fluid is the fluid surrounding the fetus within the amniotic sac. It serves several important functions, including allowing room for fetal growth and movement, ingestion for development, and protecting the fetus from trauma. Abnormal amounts of amniotic fluid can be diagnosed through ultrasound measurement of the amniotic fluid index or deepest vertical pool. Polyhydramnios, an excessive amount of fluid, can cause complications for both mother and fetus like preterm delivery. Oligohydramnios, a deficiency of fluid, increases risks like fetal distress, deformities, and malformations. Management depends on the cause, gestational age, severity, and fetal well-being and may include increased monitoring, induction of