This document provides an overview of pleural effusions, including:
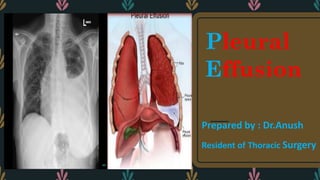
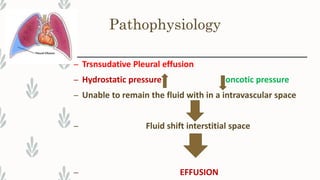
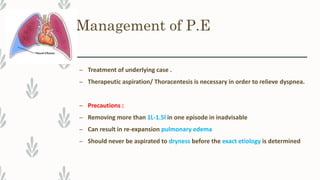
- Pleural effusions occur when there is an abnormal accumulation of fluid in the pleural space, which can be caused by changes in hydrostatic or oncotic pressures or permeability of the pleura.
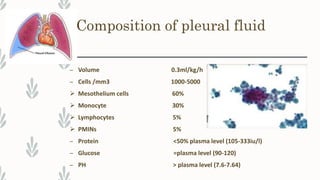
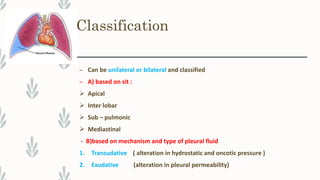
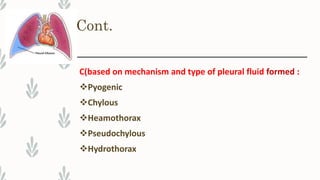
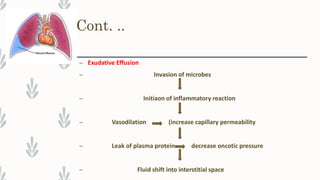
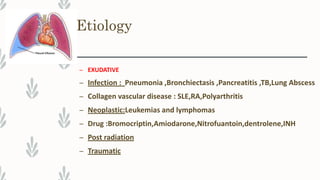
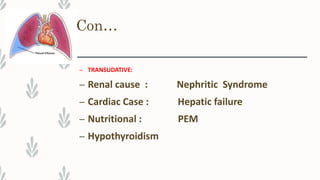
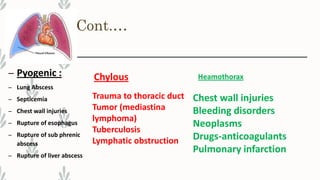
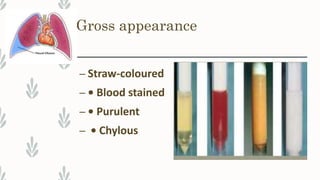
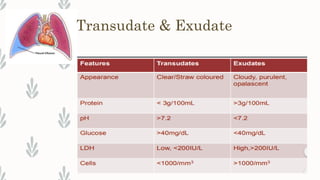
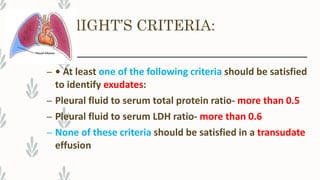
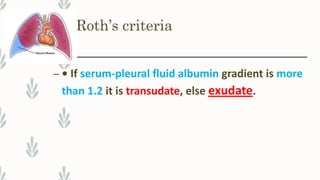
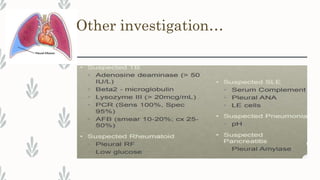
- Pleural effusions are classified as transudative or exudative based on their mechanism and fluid composition, and can be further categorized by location, cause, and appearance.
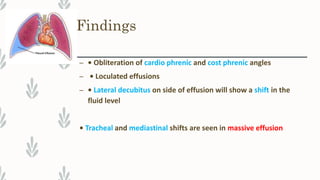
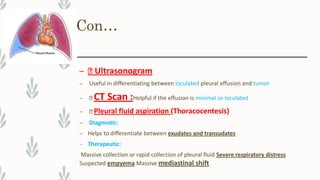
- Clinical features vary depending on the size of the effusion but may include pain, cough, dyspnea, and physical exam findings of reduced breath sounds and dullness to percussion. Diagnosis involves imaging, fluid analysis, and applying diagnostic criteria to