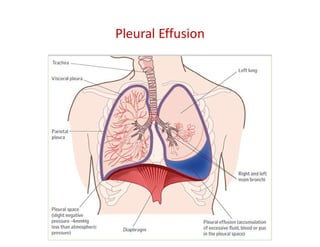
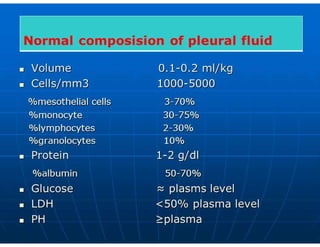
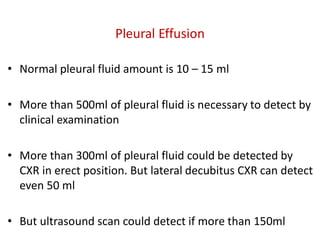
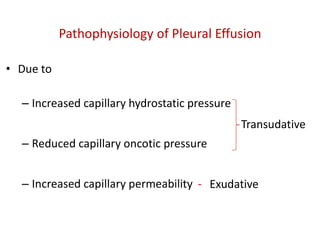
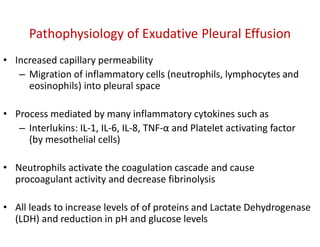
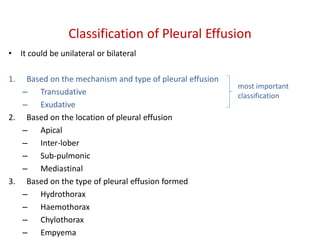
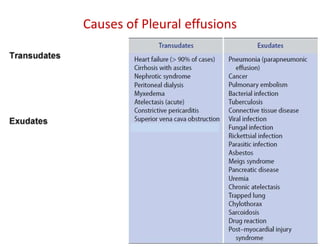
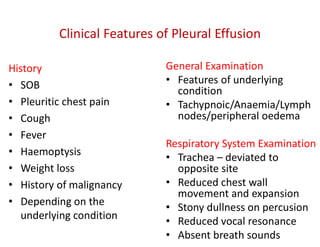
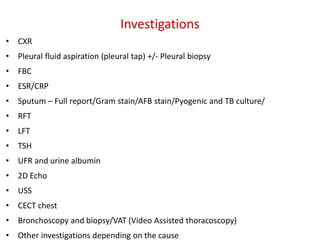
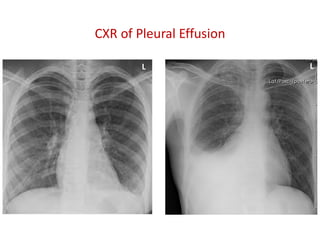
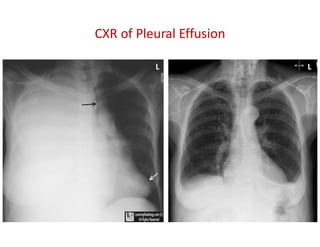
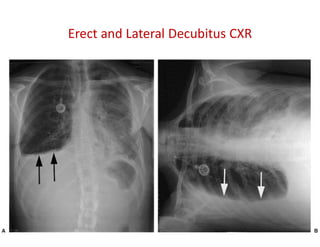
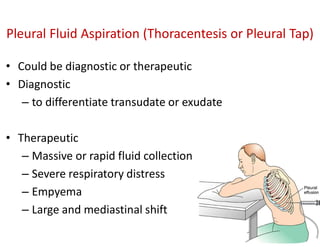
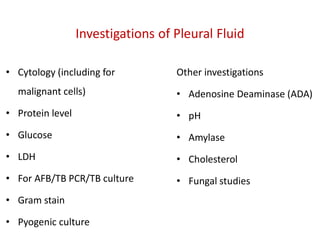
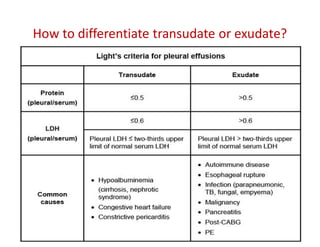
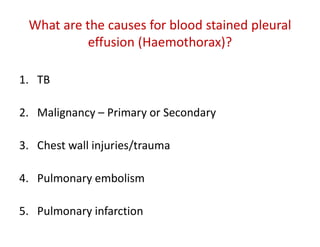
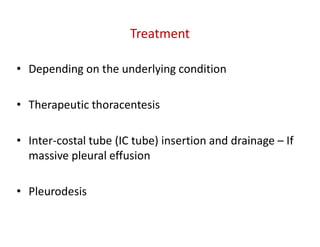
Pleural effusion is the abnormal accumulation of fluid in the pleural space, categorized as transudative or exudative based on its underlying mechanisms. Diagnosis involves clinical examination, imaging, and pleural fluid analysis, including tests for cell count, protein levels, and various cultures. Treatment varies depending on the cause and may include therapeutic thoracentesis, drainage through inter-costal tubes, or pleurodesis.