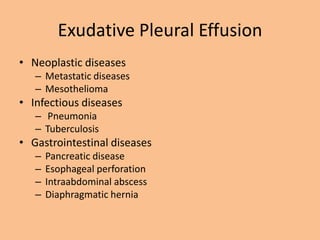
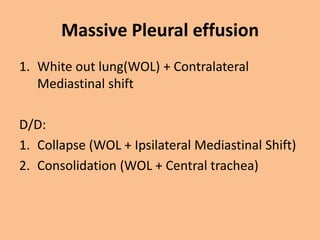
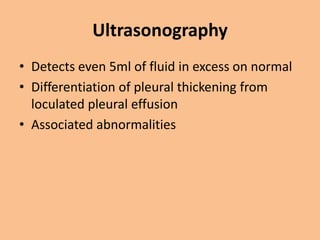
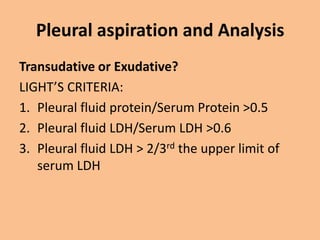
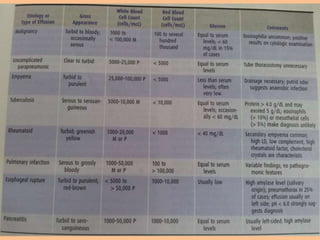
A 65-year-old male smoker presented with left-sided chest pain and difficulty breathing for 2 weeks and was found to have a left pleural effusion secondary to tuberculosis based on symptoms, examination findings showing dullness and absent breath sounds on the left side, and imaging showing pleural effusion on the left.