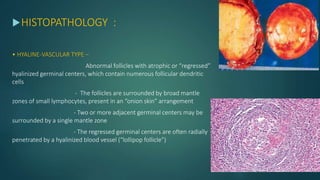
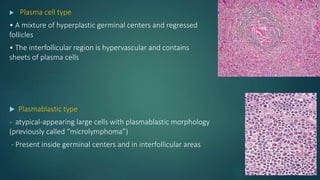
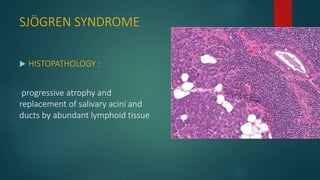
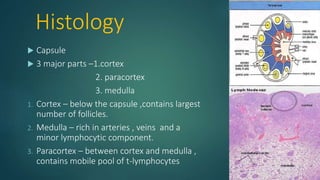
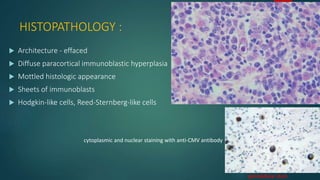
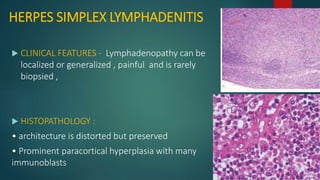
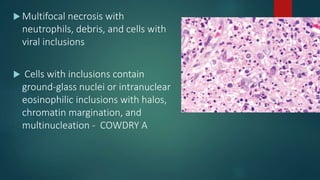
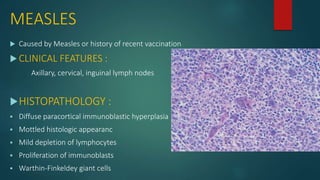
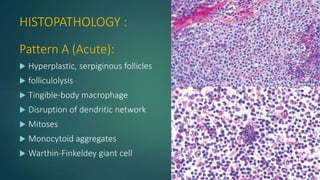
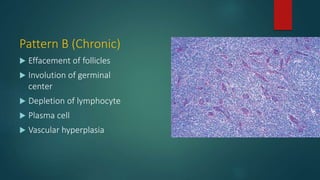
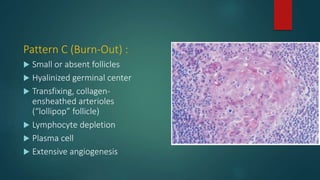
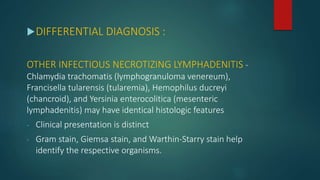
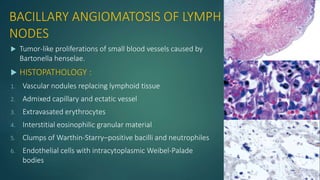
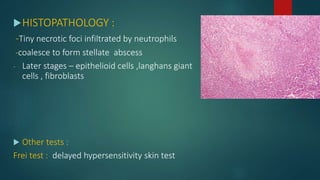
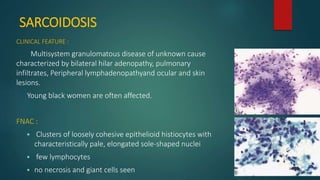
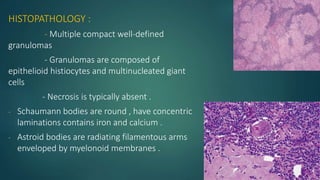
This document discusses the histology and classification of non-neoplastic lymphadenopathy. It begins by describing the histology of lymph nodes, including the capsule, cortex, paracortex, and medulla. Guidelines for examining lymph nodes through grossing, fixation, sectioning and staining are provided. Non-neoplastic lymphadenopathy is classified into lymphadenitides caused by various infectious agents like viruses, bacteria, mycobacteria, fungi and protozoa, and lymphadenopathies associated with clinical syndromes. Specific conditions are then discussed in detail, including their etiology, clinical features, histopathology, special staining, and differential diagnosis.













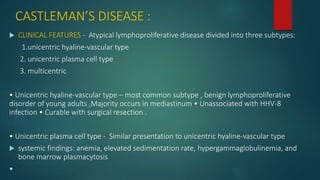
![ Multicentric - Middle-aged and elderly adults , generalized peripheral lymphadenopathy,
hepatosplenomegaly, frequent fevers, and night sweats , Strongly associated with
immunosuppression (e.g., HIV) and HHV-8 infection
associated malignancy (polyneuropathy, organomegaly, endocrinopathy, monoclonal
gammopathy, and skin changes [POEMS] syndrome, Kaposi sarcoma, Hodgkin and non-
Hodgkin lymphoma](https://image.slidesharecdn.com/nonneoplasticlymphadenopathy2-161119181046/85/Non-neoplastic-lymphadenopathy-84-320.jpg)