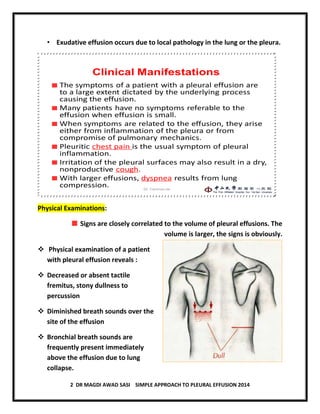
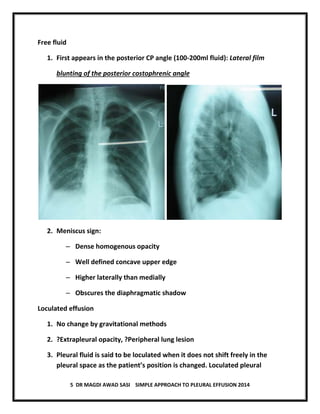
The document discusses pleural effusion, including its normal physiology, pathogenesis, clinical manifestations, aetiology, investigations, and medical management. Pleural effusion occurs when fluid formation in the pleural space increases or absorption decreases, causing fluid accumulation. Effusions can be transudative or exudative. Investigations include chest x-ray, ultrasound, and thoracentesis for diagnostic and therapeutic purposes. Management involves treating the underlying cause, therapeutic thoracentesis for symptom relief, and procedures for recurrent or complicated effusions.