What is normal blood loss | Puberty menorrhagia
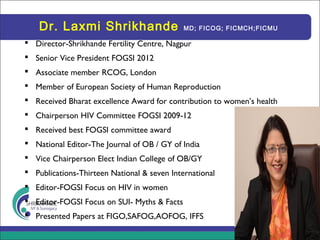
- 1. Dr. Laxmi Shrikhande MD; FICOG; FICMCH;FICMU Director-Shrikhande Fertility Centre, Nagpur Senior Vice President FOGSI 2012 Associate member RCOG, London Member of European Society of Human Reproduction Received Bharat excellence Award for contribution to women’s health Chairperson HIV Committee FOGSI 2009-12 Received best FOGSI committee award National Editor-The Journal of OB / GY of India Vice Chairperson Elect Indian College of OB/GY Publications-Thirteen National & seven International Editor-FOGSI Focus on HIV in women Editor-FOGSI Focus on SUI- Myths & Facts Presented Papers at FIGO,SAFOG,AOFOG, IFFS
- 2. Puberty menorrhagia Dr Laxmi Shrikhande Director-Shrikhande Fertility Clinic
- 3. Abnormal Menstrual Bleeding Pediatr Ann. 2015 Sep;44(9):e218-22
- 4. What is normal blood loss ? • there is considerable cycle variability in the adolescent years. • Regular ovulatory menstrual cycles occur every 21 to 35 days and last up to 7 days, with an average blood loss of 25 to 69 mL. • Many patients complain of menstrual problems that actually fall within normal variations. In the first year after menarche, 50% of cycles are anovulatory, but 80% still fall in the normal range for duration. By the third year of menarche, 95% of menstrual cycles fall into this range. • Charting the menstrual flow on a calendar can be helpful to clarify normal versus abnormal cycles. Cycles that fall outside of the norm should be evaluated for underlying pathology.
- 5. History • Amenoorrohea followed by prolonged HMB-PCOS/ anovulatory cycles • Sexual history • Bleeding diethesis • Medications • Renal disease • Liver disease • Family H/O bleeding disorder
- 6. Detail menstrual history • age at menarche • timing, duration, and quantity of her uterine bleeding. • cramping and/or clots • should address psychosocial stressors, • weight changes, • eating and • exercise habits, S trickland J, Gibson EJ, Levine SB. Dysfunctional uterine bleeding in adolescents. J Pediatr Adolesc Gynecol. 2006; 19(1):49-51. Effective history taking from an adolescent requires particular skills and sensitivities
- 7. Physical exam-D/D guided • Haemodynamic status-acute / chronic • Degree of anaemia • Features of bleeding diethesis • Features of PCOS / BMI • Features of other endocrinopathies • P/S & P/V if sexually active
- 8. Objective definition • Prolonged –more than 7 days bleeding or • Excess blood loss > 80 ml / menstrual cycle • Patient comes with diagnosis..You need to find out the cause
- 9. aetiology • HPO dysfunction 50 %-anovulatory cycles-est hyperplasia • Blood dyscrasias 20 % -coag disordes , thrombocytopenic purpura,Von Willebrand’s disease,leukemia • PCOD 10-12 % • Hypothyroidism 4 % • Genital tuberculosis 4% • Liver disorders • Feminizing ovarian tumors-granula cell and theca cell tumors • Adrenal hyperplasia
- 10. causes • While there are multiple causes for abnormal uterine bleeding in adolescents, the most likely cause is dysfunctional uterine bleeding (DUB) due to an immature hypothalamic-pituitary-ovarian (HPO) axis, causing anovulatory cycles and irregular bleeding • Before the diagnosis of immature HPO axis can be assumed, more serious disorders must be ruled out Matytsina LA, Zoloto EV, Sinenko LV, Greydanus DE. Dysfunctional uterine bleeding in adolescents: concepts of pathophysiology and management. Prim Care Clin. 2006; 33(2): 503-515 A COG Committee on Practice Bulletins—Gynecology. ACOG practice bulletin: management of anovulatory bleeding. Int J Gynaecol Obstet. 2001;72(3):263-271.
- 11. Anovultion is the major cause • 74.28% of cases of puberty menorrhagia were due to anovulatory dysfunctional uterine bleeding. • Chaudury et al reported 71%6, Roychowdhury 61.5%7, Neinstein 95%8 of cases of puberty menorrhagia as being due to anovulation due to immaturity of hypothalamic pituitary ovarian axis. Chaudhury S, et el Indian medical journal 2007; 101(5); 161-64. Roychowdhury J,et el A study to evaluate the ethiological factors and management of puberty menorrhagia OJHAS VOL 7 Issue 1; (2008 Jan-Mar) Online journal of health and allied sciences. Neinstein LS Menstural problems in adolescents Med Clin North Am 1990; 74: 1181-90. J. Med. Sci. (Peshawar, Print) January 2012, Vol. 20, No. 1: 15-18
- 12. PCOS in adolescence • Menstrual disturbance is likely to be the main issue for adolescents with PCOS but the established long- term risks of obesity, subfertility and diabetes as well as the possible risks of endometrial hyperplasia and carcinoma (Hardiman et al., 2003) and cardiovascular disease (recently reviewed by Rajkowha et al., 2000) and breast cancer (Balen, 2001) require consideration.
- 13. Differential Diagnosis • Immature HPO-anovualtory cycles – 1 yr after menarche 85 % / 4 yr after menarche 44 % • Bleeding Diethesis • PCOS-5-10 % endometrial hyperplasia • Other Endocrinopathies-hypo/hyper thyroid/ cushing • Pregnancy and related conditions-many r sexually active • Duplication of Mullerian system • Polyps and Fibroids • Pelvic infections • Medications-hormones / antidepressant/anticoagulant
- 14. Bleeding disorders in South east asia • The majority of studies in the west report von Willebrand disease as the most common inherited bleeding disorder leading to menorrhagia whereas studies in South East Asia have found platelet function disorders as the leading inherited bleeding disorder in women with menorrhagia Nazli H, Nusrat hassan, Tasneem farzana, Tahir Sultan Shamsi Adolescent menorrhagia due to platelet disorder JPMP 1/5/52011.
- 15. Investigation • UPT • CBC • USG • Bleeding disorder • Thyroid function test / PRL • PCOS tests if needed • Pelvic USG-PCOD fibroids
- 16. Is USG needed in initial evaluation ?? • retrospective chart review of 230 patients <18 years old presenting with AUB to the gynecology clinic • The most common diagnosis in both the ultrasound group and non- ultrasound group with AUB due to an immature HPO axis. • Of the patients who received an ultrasound, 72.4% had normal findings, incidental findings were identified in 17.9% and PCOS morphology in 6.4%. • Structural causes of AUB were found in only 2 (1.3%) of the adolescents imaged. • No patient had a change in her AUB management plan due to ultrasound findings. • pelvic ultrasound is not required in the initial investigation of AUB in the adolescent population J Pediatr Adolesc Gynecol. 2016 Oct 6. pii: S1083-3188(16)30206-6
- 17. Lab work • ACOG recommends that all patients younger than 18 who present with abnormal uterine bleeding be screened for coagulation disorders, particularly von Willebrand disease, as this disorder has a prevalence of 1% and is the most common disorder that causes menorrhagia at menarche. • Screening for such disorders should include a partial thromboplastin time, prothrombin time, and assessment of platelet function, plasma von Willebrand factor (VWF) antigen, and plasma VWF activity (ristocetin cofactor activity). ACOG Committee on Adolescent Health Care. ACOG Committee Opinion No 349, November 2006. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Obstet Gynecol. 2006;108(5):1323-1328. ACOG Committee on Practice Bulletins—Gynecology. ACOG practice bulletin: management of anovulatory bleeding. Int J Gynaecol Obstet. 2001;72(3):263-271.
- 18. Bleeding disorders • Young girls with blood coagulopathies are at a high risk of abnormal bleeding with the onset of menarche, bleeding is usually heavy causing anaemia and may require blood transfusion. • Claessen et al found 20% of cases of menorrhagia to be due to primary coagulation disorders.13. • In our study 4(11.4%) patients had coagulation defects. Platelet function defects are an important cause of menorrhagia. • Saxena14 et al found platelet function disorder in 83% of women with menorrhagia due to coagulation defects. Claessens CA, Cowell CA Acute adolescent menorrhagia American journal obstet Gynaecol 1981; 139(3); 277-80. Saxena R, Gupta M, Gupta K, Kashyap R, Choudry VP Inherited bleeding disorder in Indian Women with menorrhagia Haemophilia 2003; 9: 193-96. J. Med. Sci. (Peshawar, Print) January 2012, Vol. 20, No. 1: 15-18
- 19. Frequently diagnosed bleeding disorders • Von Willebrand disease • Mild platelet function disorders • Mild factor deficiencies-eg factor XI
- 20. Criteria prompting evaluation of bleeding disorders • Personal H/O->/ 1 of the following sym – Epistaxis-> 10 min requiring medical attention – Spontaneous bruising > 2 cm / minor wound bleeding > 5 min – Bleeding from oral cavity/ GIT without obvious lesiaon – Prolonged / excessive bleeding after surgery – Hemorrhage requiring BT • Family H/O – H/O bleeding disorders – Significant bleeding complication not yet investigated • HMB since menarche • Hge from corpus luteum
- 21. Bleeding disorder investigations • 1st line- – CBC/ PS/ APTT / PT / TT – Ferritin / KFT / LFT /TSH – VWF-Ag , VWF-Rco-ristocetin cofactor activity • 2nd line – Repeat VWF Ag, VWF-Rco-F VIII – Platelet function tests • 3rd line- • Factor assays-II, V,VII, XI, XIII • Further sub specialised tests-in consultation with hematologist
- 22. Mgt aim • Contol menorrhagia • Prevent or treat anaemia • Prevent recurrence • Treat the cause
- 23. management Determining factors for treatment- • Underlying etiology • Patient’s need for contraception • Her adherence / compliance capabilities • Acceptability of adverse effects / costs • There is significant overlap in the mgt of pts with and without bleeding disorders Management of DUB in the adolescent is medical in almost all circumstances
- 24. Multiple modalities • NSAIDS • Antifibrinolytics • Hormonal • DDAVP • Replacement of missing coagulation factor
- 25. 1st line-non hormonal • NSAIDS-ibuprofen, Naproxen, Mefenamic acid • Antifibrinolytics-trenexamc acid / VWF / zpfd / • First line treatment in mild cases is tranexamic acid and NSAIDS during the menstrual cycle9. Tranexamic acid is effective, safe, the bioavailability is 35% which requires administration of at least 1 gm 4- 6 hourly10 Royal college of obstetrician and gynecologists The initial management of menorrhagia, RCOG evidence based clinical guidelines No. 1 London 1999. Lethaby A, Farquhar C, Cooke l Antifibrinolytic for heavy menstrual bleeding The Cochrane library issue 1-2003.
- 26. Mild DUB-hemodynamically stable • Hb > 10 gm % • COCP / progesterone • May increase dose to BD and then taper • Follow up with iron supplementation
- 27. Combined hormonal contraceptive • OCP-cyclic/ continuous- adolescents prefer extended cycles (84/ 7) • Transdermal patch • Vaginal ring
- 28. COC • Oral contraceptive pills taper using monophasic pills can also be given, 4 pills evenly spaced per day for 4 days, 3 pills per day for 3 days, 2 pills per day for 2 days and 1 pill /per day for 2 months without taking the placebo pill11. Linda M, Szymanski, Kimberly B Abnormal uterine bleeding, The John Hopkins manual of Gynecology and obstetrics Third edition page 417-428 Lippincote Williams and wilkins
- 29. Progestin therapy • Oral- – primolute N-effective but poorly tolerated – Deviry-cyclical t/t for hyperplasia • Long acting injectables-DMPA / NET-EN • Subcutaneous progestins-Etonogestrel implant – Impact on bone density – Irreg bleeding and ameno – Possibility of wt gain • LNG-IUS
- 30. Different dosing regimens are in practice •NETA 5-10 mg, generally administered in luteal phase from day 15/19 to day 26 in anovulatory cycles •Recently an increase in the duration and dosage has been investigated in patients with ovulatory dysfunctional uterine bleeding1 •Administration of oral progestogens from day 5 to day 26 of the cycle produced a significant reduction in bleeding1 Acute severe anovulatory bleeding: •High dose NETA 15 mg & treatment should continued for 3 weeks, tapering the dose after 7-10 days Norethisterone acetate (NETA) – Dosing Regimens Lethaby et al., The Cochrane Library 2008, Issue 1 In studies, Norethisterone progestogens were more effective in the treatment of dysfunctional uterine bleeding than dydrogesterone. (Am. Med. J. 1 (1): 23-26, 2010)
- 31. Advantages of Micronized formulations of Norethisterone acetate controlled release
- 32. Smartinor CR (Norethisterone acetate controlled release micronised tablets ) in Puberty Menorrhagia I Norethisterone acetate controls bleeding and normalizes menstrual cycle by the following actions: Effects on Uterus: Binds to progesterone receptors in the endometrium and brings synchronous secretory changes in estrogen primed endometrium Promotes regrowth of the endometrium over irregularly denuded surfaces due to its weak estrogenic action Styptic effect on uterine hemorrhage: Checks bleeding by constriction of uterine blood vessels (like a hemostatic agent) Used for the management of acute bleeding as well as for the prevention of recurrence. Beneficial in both ovulatory and anovulatory DUB.
- 33. progesterones • Progesterones alone are generally effective but can be used in combination with estrogen. • Progesterone can be used cyclically in two different treatment protocols: as a short course during the luteal phase and a relatively longer course lasting 21 days from day 5 of the cycle. • Heavy bleeding can be treated with (1) oral Medroxyprogesterone 10 mg three times /day for 14 days. (2) Medroxyprogesterone acetate injection (Depo Provera) 150 mg intramuscularly every 12 weeks. (3) Progesterone can also be used for medical curettage, in the form of norethisterone acetate 20-30 mg daily for 3 days to arrest haemorrhage. • It may then be continued at a lower dose for up to 21 days. Withdrawal bleeding will occur on stopping the treatment that ceases in 4-5 days
- 34. Side effects of progesterone only therapy • need for long-term oral medication and the possibility of unwanted `pre- menstrual symptoms’ • androgenic effects (depending on the progestogen used), such as acne and hirsutism; irregular breakthrough bleeding and a change in carbohydrate tolerance and lipid balance. • Depo-Proveraâ will induce amenorrhoea in 50% of users at 1 year and break through bleeding in 15±20% • The Mirenaâ intrauterine implant system (IUS) releasing 20 mg of levonorgestrel/day (LNG-IUS 20) is a highly effective long-term treatment for both ovulatory and anovulatory DUB (Anderson and Rybo, 1990). • Irregular `breakthrough' bleeding is the main unwanted effect of all progestogen preparations and the main reason why women choose to discontinue these preparations, despite their other advantages.
- 35. Moderate hb 10-12 • Mostly outpatient • The treatment typically involves hormonal therapy to stabilize endometrial proliferation and shedding. • The choice of agent(s) depends, to some extent, upon how heavily the patient is bleeding. • Girls with moderate DUB should be provided with iron supplementation. • Another regimen states that OC pills be taken 3 times per day until the bleeding ceases (usually within 48 hours), then tapered to twice daily for 5 days, and then decreased to once daily to complete 21 days of hormone therapy. • R imsza ME. Dysfunctional uterine bleeding. Pediatr Rev. 2002;23(7):227-233.
- 36. Severe bleeding-hemodynamically unstable • Hb < 8 gm % / severe bleeding • Hospitalization • Fluid and blood • Conjugated estrogen 25 mg IV 4-6 hrly (upto 48 hrs) till bledding stops • Add progesterone or COCP • COCP containing 30-35 Ug EE orally every 4-6 hrs till bleeding stops and taper to OD over 10-14 days
- 37. Anovulatory cycles-acute bleeding • IV premarin 25 mg 6-8 hrly x 24-48 hrs followed by est for 21 days with prog added for 10 days for 3-6 cycles- • Current trend is to give IV trenaxemic acid 1 gm with 25 mg of est and then continue with E and P as mentioned above
- 38. Multidisciplinary approach • Involve hematologist • Surgical intervention rarely required-D & C, foley ballon temponade in refractory / life threatning HMB
- 39. Role of Diosmin in Puberty Menorrhagia Apart from Hormonal imbalance increased Capillary fragility and increased PGE 2 secretion can also be a contributing causes for Puberty menorrhagia.1 Lymphatic drainage is underdeveloped in human endometrium. Increased bleeding causes accumulation of debris and tissue products which lymphatic system is unable to cope. Vasoprotectors like bioflavonoid (Diosmin) can play a vital role in controlling the bleeding given along with hormonal treatment , non hormonal treatment. Diosmin is a naturally occurring flavonoid glycoside . Widely used for more than 40 years worldwide with good efficacy and safety profile. In Puberty Menorrhagia Dose is 900 mg daily, until the normalization of menstrual cycle. 1. International Journal of Gynecology and Obstetrics , Volume 89 , Issue 2 , 156 - 157
- 40. How can Diosmin be useful in Puberty Menorrhagia Diosmin Micronized and 100% pure diosmin formulation should be preferred over the conventional formulations of DIOSMIN in the market for better results . Micronization of Diosmin increases the surface area available for intestinal absorption, thus increases the bioavailability Diosmin.
- 41. Diosmin in Menorrhagia Summary of Clinical Trials 100% Pure micronized diosmin is a potent , gentle, non-hormonal treatment in cases of menorrhagia , with or without hormonal therapy. Summary of Clinical trials i. Pure Diosmin reduces amount of bleeding upto 51.9% ii. Reduces duration of bleeding by 2.6 days iii. Relieves dysmenorrhea score by 53.1% iv. Normalizes menstrual cycle by 82%. v. Effective in Functional gynaecological bleeding in 88-98% patients. vi. Safe and well tolerated In Puberty Menorrhagia Dose is 900 mg daily, until the normalization of menstrual cycle Source : Int J Gynaecol Obstet. 2005 May;89(2):156-7, Gobet A. Med. Prat. 1978; (1-2): 713-14
- 42. FOLLOW-UP AND LONG-TERM CARE • After treatment is initiated, patients should be seen at regular intervals • Long-term management depends on the anemia and the desire for contraception. • Most experts recommend continuing hormonal therapy for at least 6 months. • After therapy is discontinued, the patient should still be followed to ensure regulation of menstruation.
- 43. Must do • All pts iron deficiency assessed and treated • No iron preparation is more effective than other • 150-200 mg elemental iron/dayin 1-3 divided doses • Empty stomach with glass of orange juice • Duration of t/t is 3 months beyond normalisation of HB to replenish iron store
- 44. conclusion • Abnormal menstrual bleeding in adolescents can be caused by a number of conditions, the most common cause is immaturity of the hypothalamic pituitary ovarian axis. • Bleeding disorders are another. • Assessment of each case with thorough history, physical examination, and laboratory investigations are crucial in reaching the diagnosis. • Once a proper diagnosis is made, counseling of the patient and her parents, follow up and long term therapy in some cases is required.
- 45. Dr. Laxmi Shrikhande Shrikhande IVF & Surrogacy Center Ph-96234 59766 / shrikhandedrlaxmi@gmail.com
- 46. 'Spiritual blossoming' simply means blossoming in life in all dimensions. Being happy, at ease with yourself and with everybody around you. Sri Sri Ravi Shankar The Art of Living
- 47. coagulopathy • Young girls with blood coagulopathy are at a high risk of abnormal bleeding with the onset of menarche. Bleeding is usually heavy, causing anaemia and may require blood transfusion. Among the inherited bleeding disorders platelet defects are the most common causes of puberty menorrhagia2 Phillipp CS, Faiz A, Dowling N, Dilley A, Micheals LA et al Age and prevalence of bleeding disorders in women with menorrhagia Obstet gynaecol 2005; 105: 61-68.
- 48. Mild DUB • Mild Uterine Bleeding (Hgb >12 mg/dL) Management of mild abnormal bleeding consists of observation and reassurance. If hemoglobin (Hgb) concentration is normal (>12 mg/dL), girls with mild DUB should be asked to keep a menstrual calendar and can be given the option to avoid treatment with hormonal therapy. They should follow up in 3 to 6 months, unless bleeding becomes more severe, in which case they should be seen acutely.
- 49. When to admit • Hospitalization is necessary for patients who are hemodynamically unstable, who have low Hgb concentration (<7 mg/ dL), or who have symptomatic anemia.8 E mans SJ. Dysfunctional uterine bleeding. In: Emans SJ, Laufer MR, Goldstein DP, eds. Pediatric and Adolescent Gynecology. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:270. • Heavy active bleeding and Hgb lower than 10 mg/dL are also considered by some to be an indication for hospitalization. • If the Hgb is between 8 and 10 mg/dL, and the patient is hemodynamically stable, and the patient and family are reliable and can maintain close telephone contact, home management may be possible with daily monitoring
- 50. Acute bleeding • For patients who can tolerate oral intake, therapy typically includes a monophasic combination OC pill with 50 g estradiol and 0.5 mg norgestrel (eg,μ Ovral, Ogestrel) or 50 g estradiol and 1 mgμ norethindrone (eg, Ovcon 50), administered according to various schedules. A common schedule is to take it 4 times a day until bleeding is controlled, then wean to 3 times daily for 3 days, and then to twice daily to complete a 21day course of pills.8 Then the patient starts a new pack of pills (without using the placebo pills). For patients who
- 51. Desmopressin acetate DDAVP • Induces secretion of VWF from endothelial lining in increased VWF and F VIII • VWF • Hemophilia • PFD • 77 % effective • Side effects-tachyphylaxis / fluid retention/ hyponatremia
- 52. Desmopressin for Van Willebrand’s syndrome • Desmopressin analogue of arginine vasopressin is given IV or nasal spray 1.5 mg/ml-total 150-300 mg in 30 ml diluted
- 53. • Take he opportunity to educate girl on life style issues • Reassure her that 80 % menstrual problems falls in normal range • HPO axis immaturity is the major cause • 10 % do need coagulation evaluation
- 54. summary • Adolescents with gynaecological problems require a degree of privacy and sensitive handling, as many of the gynaecological problems encountered relate to intimate body functions at a time when the individual is maturing sexually and having to deal with issues that are embarrassing and may be considered taboo
Editor's Notes
- The International Federation of Gynecology and Obstetrics and the American Congress of Obstetricians and Gynecologists support the use of new terminology for abnormal uterine bleeding (AUB) to consistently categorize AUB by etiology. The term AUB can be further classified as AUB/heavy menstrual bleeding (HMB) (replacing the term &quot;menorrhagia&quot;) or AUB/intermenstrual bleeding (replacing the term &quot;metrorrhagia&quot;). Although many cases of AUB in adolescent women are attributable to immaturity of the hypothalamic-pituitary-ovarian axis, underlying bleeding disorders should be considered in women with AUB/HMB
- Menstrual disorders are among the most common complaints of adolescents. This is in part because adolescents and their families often have difficulty understanding what normal cycles or patterns of bleeding are and in part because there is considerable menstrual cycle variability in the adolescent years.1 Regular ovulatory menstrual cycles occur every 21 to 35 days and last up to 7 days, with an average blood loss of 25 to 69 mL.2 Many patients complain of menstrual problems that actually fall within normal variations. In the first year after menarche, 50% of cycles are anovulatory, but 80% still fall in the normal range for duration. By the third year of menarche, 95% of menstrual cycles fall into this range.3 Charting the menstrual flow on a calendar can be helpful to clarify normal versus abnormal cycles. Cycles that fall outside of the norm should be evaluated for underlying pathology.
- Embarrassment about discussing menstruation, fear of disease and ignorance about available services are likely to mean that many problems are not discussed or present following maternal pressure. Alternatively, presentation with a menstrual disturbance may disguise other issues, such as those relating to contraception, pregnancy, sexually transmitted infection (STI) or even sexual assault, and the gynaecologist should ensure that the young woman is given the opportunity to raise other concern
- When an adolescent presents with the complaint of DUB, she should be asked detailed questions about her menstrual history, including the age at menarche and the timing, duration, and quantity of her uterine bleeding. The presence of cramping and/or clots can be useful information as well. Review of systems should address psychosocial stressors, weight changes, eating and exercise habits, medications, and symptoms of hyperandrogenism. Family history of bleeding disorders and menstrual history is imperative, as is a sexual history.7
- Physical examination should include vital signs and evaluate for signs of hyperandrogenism and bleeding. The Sexual Maturity Rating scale should be determined to be at the appropriate stage for the patient’s age. The nipples should be assessed for discharge. In most patients, especially those who are not sexually active, an internal pelvic exam is not necessary to evaluate the pelvic anatomy. In such patients, an ultrasound may be sufficient to evaluate for pelvic pathology.
- PCOS in adolescence PCOS appears to underlie irregular menses in up to one-third of girls (Venturoli et al., 1986). Menarche is not usually delayed, but bleeding is then persistently irregular. In adolescents, PCOS can present with primary or secondary amenorrhoea, acne, hirsutism or merely irregular periods, as set out in Table IV. Ovarian dysfunction leads to the main signs and symptoms of the PCOS and the ovary is in¯uenced by external factors, in particular the gonadotrophins and insulin, which are themselves dependent upon both genetic and environmental in¯uences. Approximately 20±33% of women of reproductive age will have polycystic ovaries on ultrasound scan (Polson et al., 1988; Michelmore et al., 1999); while perhaps 75±80% of these will have symptoms consistent with the diagnosis of PCOS. Menstrual disturbance is likely to be the main issue for adolescents with PCOS but the established long-term risks of obesity, subfertility and diabetes as well as the possible risks of endometrial hyperplasia and carcinoma (Hardiman et al., 2003) and cardiovascular disease (recently reviewed by Rajkowha et al., 2000) and breast cancer (Balen, 2001) require consideration. Obesity also compounds the clinical manifestations of PCOS and weight loss may lead to symptom improvement. PCOS may ®rst manifest in adolescence but its origins are likely to be much earlier. PCOS is associated with increased weight gain during puberty (Balen and Dunger, 1995). Genetic study of PCOS has identi®ed links with insulin secretion and action as well as increased ovarian androgen secretion). Association has been reported with common allelic variation at the variable number of tandem repeat locus (VNTR) in the promoter region of the insulin gene (Waterworth et al., 1997). This locus has been variably associated with the risk of obesity, insulin resistance and type 2 diabetes. The identi®ed association has been with the class III/III genotype, particularly in women who have anovulatory cycles and are hyperinsulinaemic (Waterworth et al., 1997; Michelmore et al., 2001).
- J Pediatr Adolesc Gynecol. 2016 Oct 6. pii: S1083-3188(16)30206-6. doi: 10.1016/j.jpag.2016.09.012. [Epub ahead of print] The utility of routine ultrasound in the diagnosis and management of adolescents with abnormal uterine bleeding. Pecchioli Y1, Oyewumi L2, Allen LM3, Kives S3. Author information Abstract STUDY OBJECTIVE: Despite the fact that most cases of abnormal uterine bleeding (AUB) in adolescence are due to an immature hypothalamic-pituitary-ovarian axis (HPO), the current approach to investigating adolescents presenting with AUB often includes pelvic ultrasound to exclude rare structural causes. The aim of this study was to determine whether an ultrasound ordered for the investigation of AUB in adolescents detects any significant anatomic pathology or alters diagnosis and management. DESIGN, SETTING AND PARTICIPANTS: A retrospective chart review of 230 patients &lt;18 years old presenting with AUB to the gynecology clinic at the Hospital for Sick Children in Toronto, Canada between January 2010 and December 2012 was completed. MAIN OUTCOME MEASURES: Findings on pelvic ultrasound and any further imaging as well as management choices for these patients were examined. RESULTS: 67.8% of the patients had ultrasound done as part of their AUB workup. The most common diagnosis in both the ultrasound group and non-ultrasound group with AUB due to an immature HPO axis. Of the patients who received an ultrasound, 72.4% had normal findings, incidental findings were identified in 17.9% and PCOS morphology in 6.4%. Structural causes of AUB were found in only 2 (1.3%) of the adolescents imaged. No patient had a change in her AUB management plan due to ultrasound findings. CONCLUSIONS: Our results strongly suggest that pelvic ultrasound is not required in the initial investigation of AUB in the adolescent population as it did not alter treatment in any of our patients.
- Laboratory work-up of adolescents with abnormal uterine bleeding should include a pregnancy test, regardless of whether the history reveals sexual activity. Once pregnancy has been ruled out, the practitioner should consider additional lab work to rule on other diagnoses in the differential based on the presenting signs and symptoms. A complete blood count may be helpful to evaluate for anemia. ACOG recommends that all patients younger than 18 who present with abnormal uterine bleeding be screened for coagulation disorders, particularly von Willebrand disease, as this disorder has a prevalence of 1% and is the most common disorder that causes menorrhagia at menarche.1,6 Screening for such disorders should include a partial thromboplastin time, prothrombin time, and assessment of platelet function, plasma von Willebrand factor (VWF)
- Mild Uterine Bleeding (Hgb &gt;12 mg/dL) Management of mild abnormal bleeding consists of observation and reassurance. If hemoglobin (Hgb) concentration is normal (&gt;12 mg/dL), girls with mild DUB should be asked to keep a menstrual calendar and can be given the option to avoid treatment with hormonal therapy. They should follow up in 3 to 6 months, unless bleeding becomes more severe, in which case they should be seen acutely.
- Progesterones alone are generally effective but can be used in combination with estrogen. Progesterone can be used cyclically in two different treatment protocols: as a short course during the luteal phase and a relatively longer course lasting 21 days from day 5 of the cycle. Heavy bleeding can be treated with (1) oral Medroxyprogesterone 10 mg three times /day for 14 days. (2) Medroxyprogesterone acetate injection (Depo Provera) 150 mg intramuscularly every 12 weeks. (3) Progesterone can also be used for medical curettage, in the form of norethisterone acetate 20-30 mg daily for 3 days to arrest haemorrhage. It may then be continued at a lower dose for up to 21 days. Withdrawal bleeding will occur on stopping the treatment that ceases in 4-5 days
- The disadvantages of oral progestogen regimens for DUB include the need for long-term oral medication and the possibility of unwanted `pre-menstrual symptoms&apos; including: bloating, edema, headache, depression and reduced libido; androgenic effects (depending on the progestogen used), such as acne and hirsutism; irregular breakthrough bleeding and a change in carbohydrate tolerance and lipid balance. The contraceptive depot preparation of medroxyprogesterone acetate (such as Depo-Proveraâ) will induce amenorrhoea in 50% of users at 1 year. For those who can accept the 15±20% rate of irregular or prolonged breakthrough bleeding, this may provide a safe and effective treatment regimen. The Mirenaâ intrauterine implant system (IUS) releasing 20 mg of levonorgestrel/day (LNG-IUS 20) is a highly effective long-term treatment for both ovulatory and anovulatory DUB (Anderson and Rybo, 1990). The system also provides reversible contraception. The Mirena has a place in the management of refractory DUB in young women but the physician should consider insertion of the device under general anaesthetic. Hysteroscopy at the same time may also be indicated to exclude (rare) intrauterine pathology if a general anaesthetic is planned. Irregular `breakthrough&apos; bleeding is the main unwanted effect of all progestogen preparations and the main reason why women choose to discontinue these preparations, despite their other advantages.
- There is a paucity of data from randomized trials regarding the treatment of DUB in adolescents. Nonetheless, there are a variety of regimens that appear to be equally effective. Patients who have complaints of heavier bleeding may have a better response to oral contraceptives (OCs) that have a combination of estrogen and progestin rather than to progestin-only preparations, as estrogen provides hemostasis. Thus, one option is to use monophasic contraceptive pills in the traditional fashion of 1 per day. Another regimen states that OC pills be taken 3 times per day until the bleeding ceases (usually within 48 hours), then tapered to twice daily for 5 days, and then decreased to once daily to complete 21 days of hormone therapy.9 Once the 21-day course is finished, patients start another pack and take 1 pill per day in the typical fashion. If bleeding recurs when the dose is decreased to once per day, twice-perday dosing may be necessary for an extended period of time. Close follow-up is essential during twice-per-day dosing. High-dose estrogen therapy can cause nausea, which may result in noncompliance. Antiemetic therapy (ie, promethazine or ondansetron) is often required before each dose of the pill.8 Progestin-only therapy is an alternative for girls with moderate DUB who cannot tolerate, dislike, or have a contraindication to estrogen therapy
- FOLLOW-UP AND LONG-TERM CARE After treatment is initiated, patients should be seen at regular intervals to ensure that their bleeding profile has improved to their satisfaction and that they are tolerating any medicines that may have been started. Long-term management depends on the anemia and the desire for contraception. Most experts recommend continuing hormonal therapy for at least 6 months. After therapy is discontinued, the patient should still be followed to ensure regulation of menstruation.
- Mild Uterine Bleeding (Hgb &gt;12 mg/dL) Management of mild abnormal bleeding consists of observation and reassurance. If hemoglobin (Hgb) concentration is normal (&gt;12 mg/dL), girls with mild DUB should be asked to keep a menstrual calendar and can be given the option to avoid treatment with hormonal therapy. They should follow up in 3 to 6 months, unless bleeding becomes more severe, in which case they should be seen acutely.
- Hospitalization is necessary for patients who are hemodynamically unstable, who have low Hgb concentration (&lt;7 mg/ dL), or who have symptomatic anemia.8 Heavy active bleeding and Hgb lower than 10 mg/dL are also considered by some to be an indication for hospitalization. If the Hgb is between 8 and 10 mg/dL, and the patient is hemodynamically stable, and the patient and family are reliable and can maintain close telephone contact, home management may be possible with daily monitoring
- For patients who can tolerate oral intake, therapy typically includes a monophasic combination OC pill with 50 μg estradiol and 0.5 mg norgestrel (eg, Ovral, Ogestrel) or 50 μg estradiol and 1 mg norethindrone (eg, Ovcon 50), administered according to various schedules. A common schedule is to take it 4 times a day until bleeding is controlled, then wean to 3 times daily for 3 days, and then to twice daily to complete a 21day course of pills.8 Then the patient starts a new pack of pills (without using the placebo pills). For patients who can take oral medications but in whom estrogen is contraindicated (eg, those with thromboembolic disease, estrogen-dependent tumors, or hepatic disease), a progestin such as norethindrone acetate (5 to 10 mg daily) or micronized progesterone (200 mg before bedtime) can be used. In patients who need intravenous treatment, conjugated equine estrogen (Premarin) may be used. In cases of severe menorrhagia unresponsive to 24 hours of hormonal therapy or in those with platelet dysfunction, nonhormonal hemostatic drugs may be used. These include the antifibrinolytic compounds, aminocaproic acid or tranexamic acid, or desmopressin, which is classically used for the treatment of von Willebrand disease.11 Treatment is continued for approximately 8 hours or until the bleeding has been controlled. Once the bleeding has been controlled and the patient can tolerate oral intake, she should be transitioned to oral hormonal therapy for maintenance.
