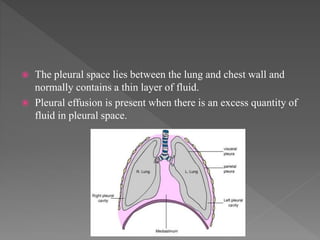
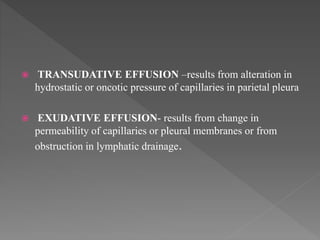
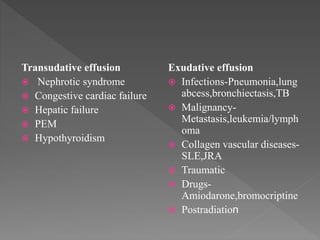
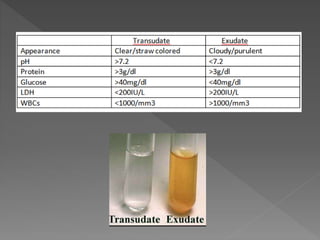
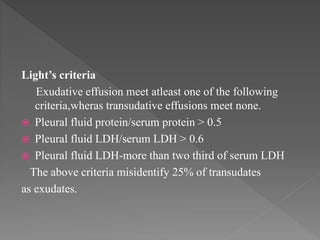
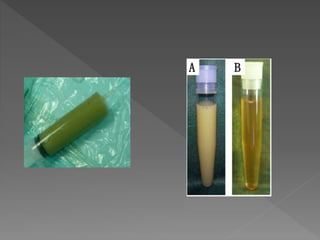
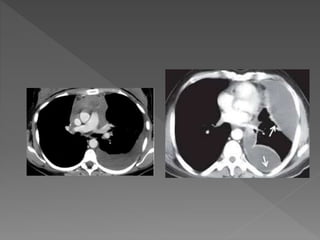
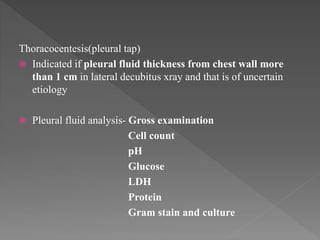
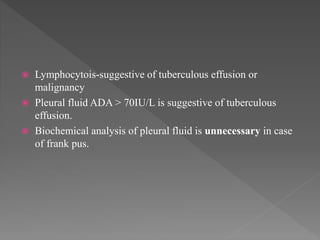
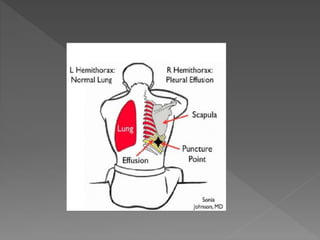
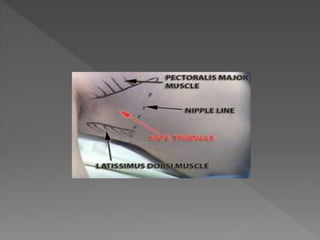
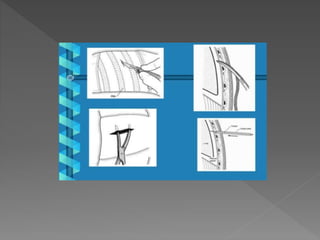
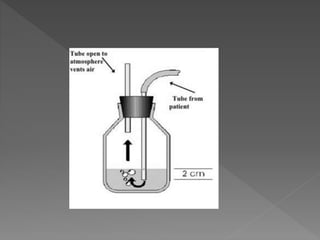
The document discusses pleural effusions and empyema. It defines pleural effusions as excess fluid in the pleural space, which can be transudative or exudative based on its cause. Empyema is defined as pus or microorganisms present in the pleural fluid. Empyema progresses through exudative, fibrinopurulent and organizational stages. Treatment of empyema involves antibiotics, chest tube drainage, and sometimes surgery.