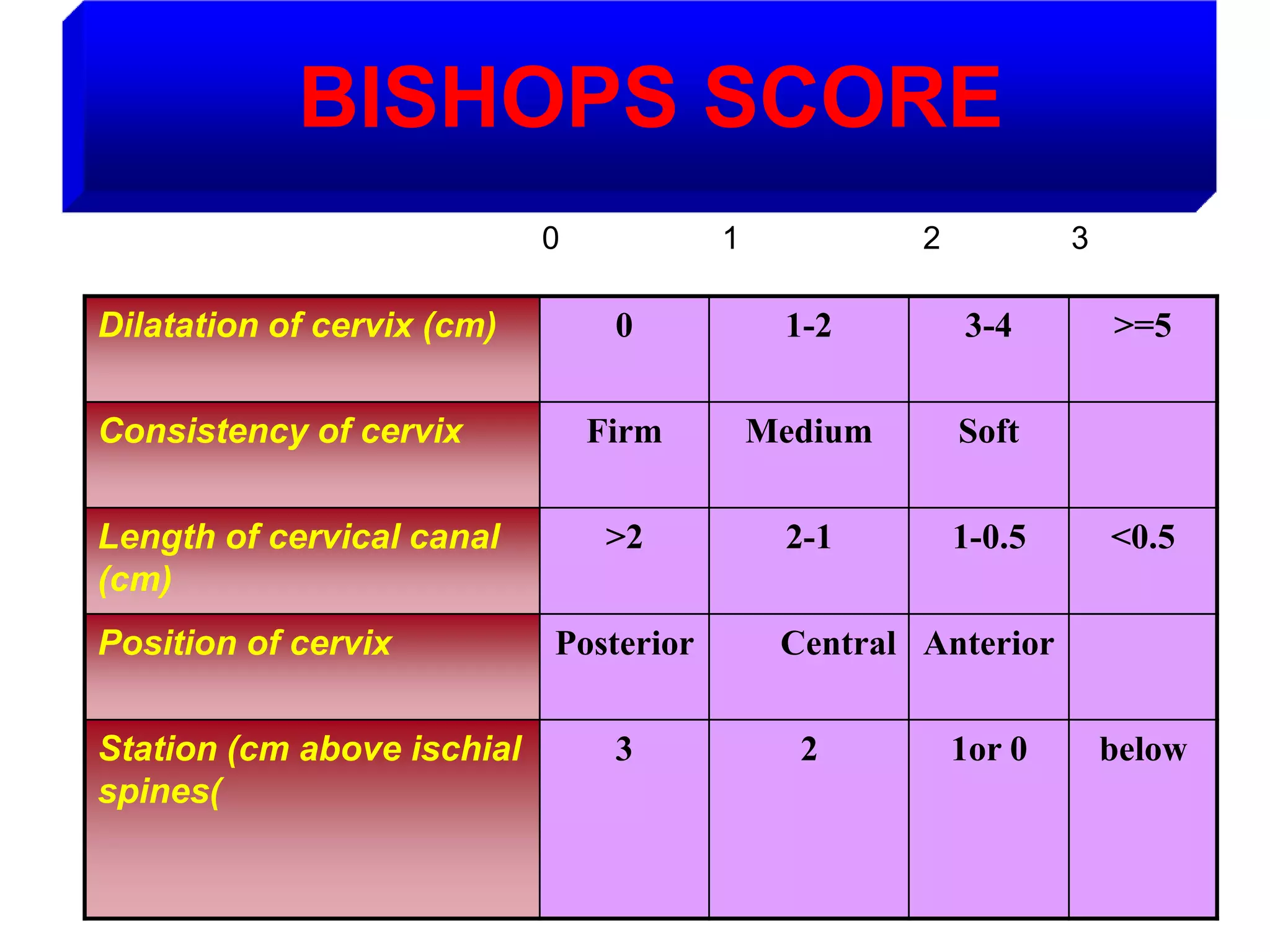
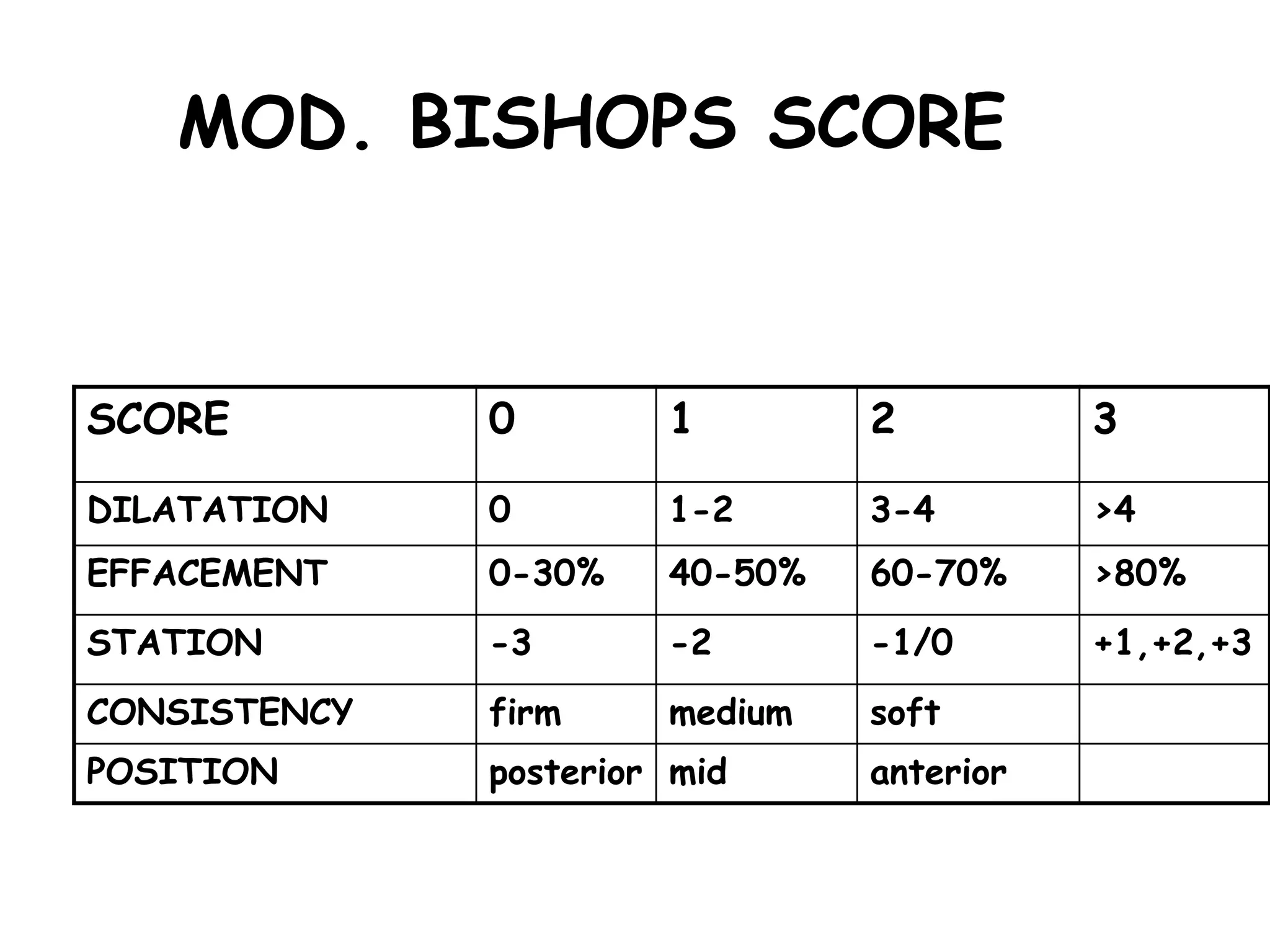
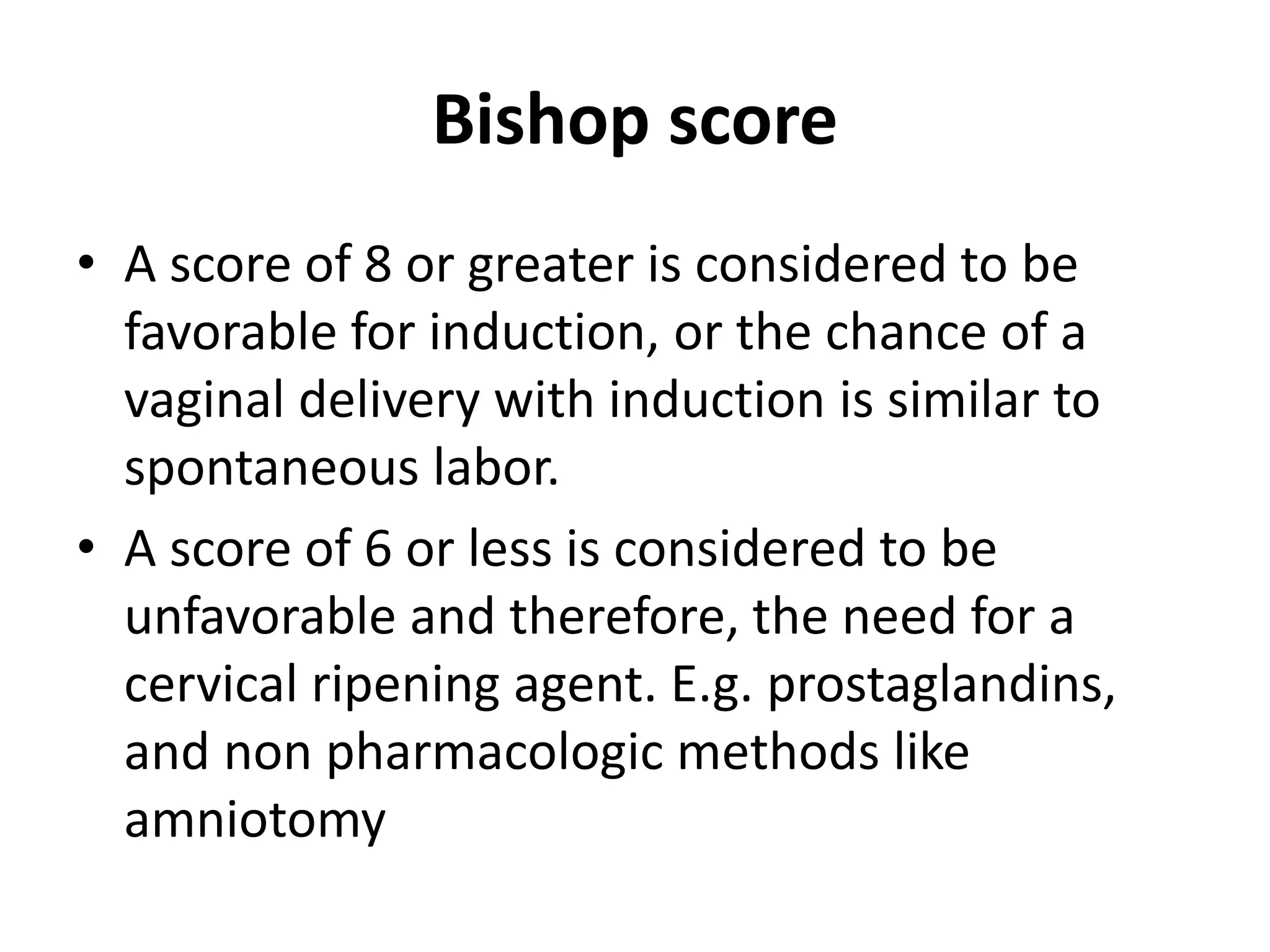
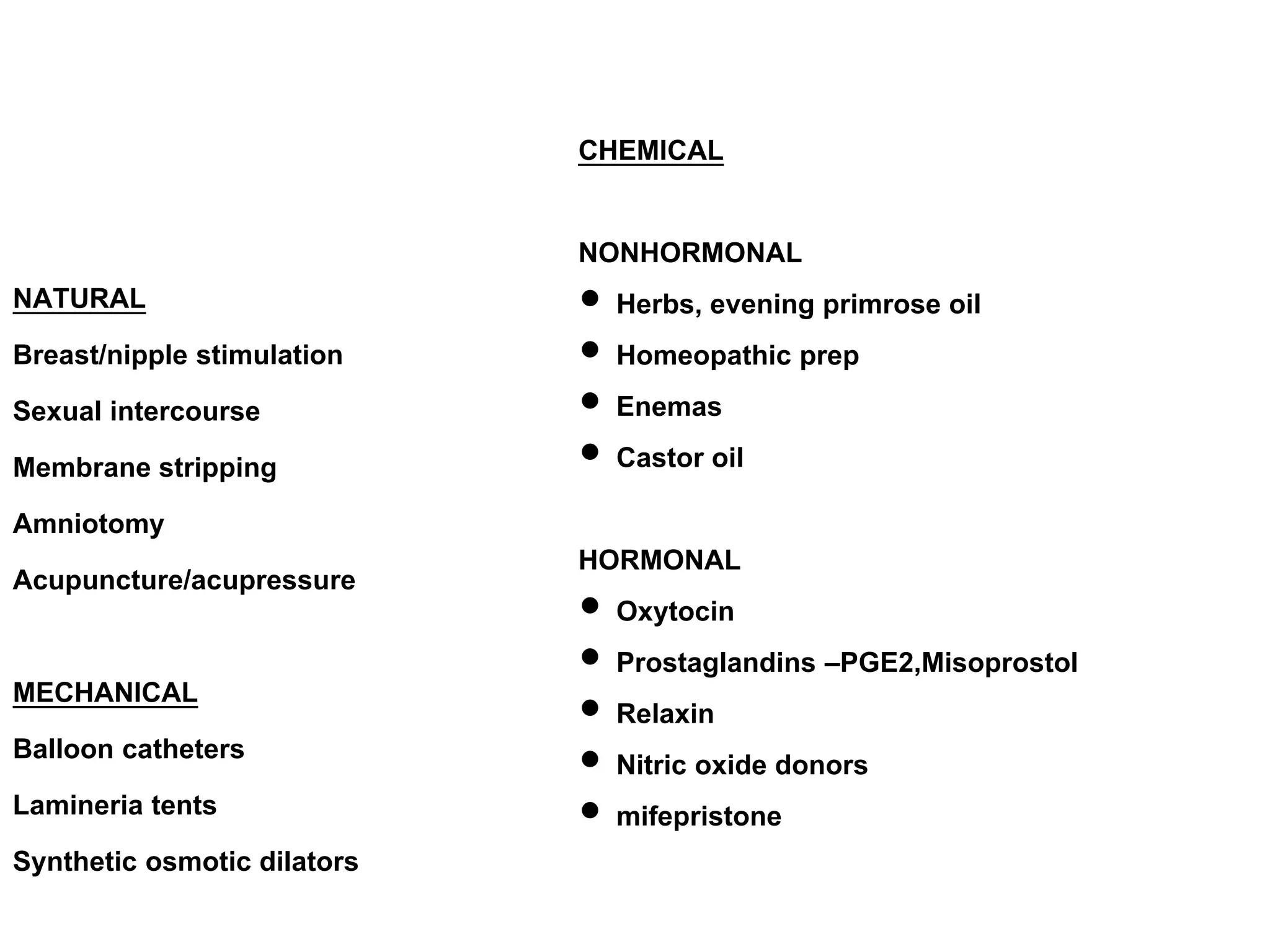
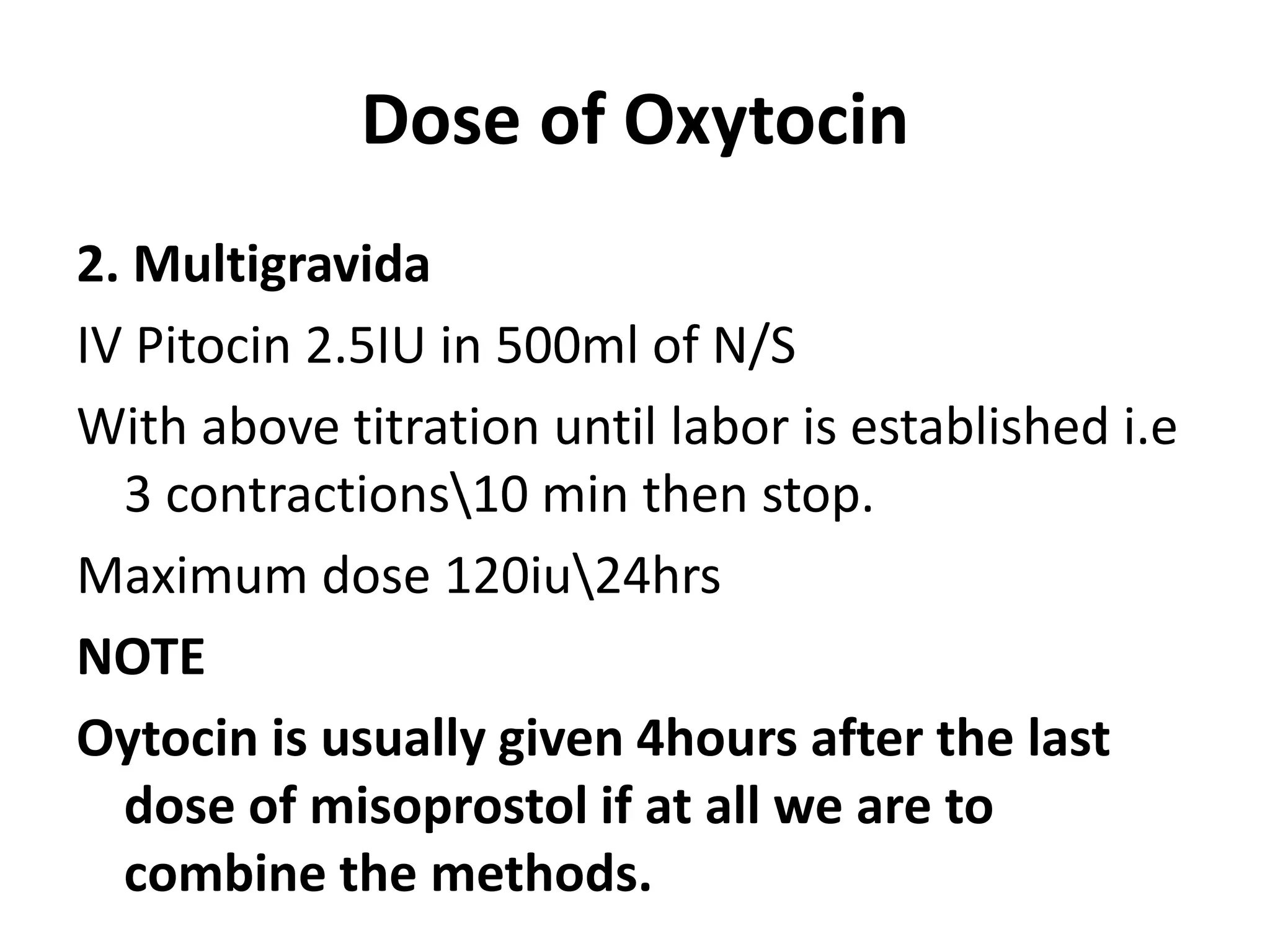
Induction and augmentation of labor involves initiating or strengthening contractions to achieve vaginal birth. Induction is done when pregnancy has reached term but labor has not begun spontaneously, while augmentation refers to stimulating an already started labor. Common induction methods include prostaglandins like misoprostol to ripen the cervix, balloon catheters, and oxytocin infusion. Indications for induction include pregnancy complications or post-dates pregnancy, while risks include failed induction and increased cesarean delivery rates. Careful patient assessment and individualizing the induction approach can help maximize benefits and minimize risks.