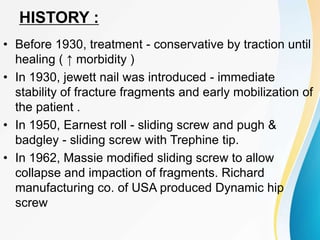
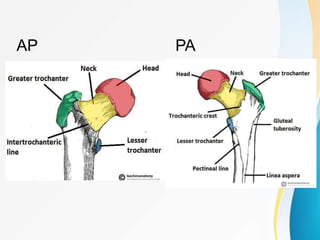
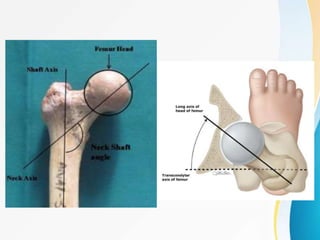
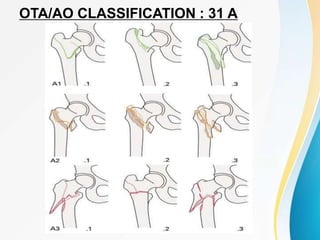
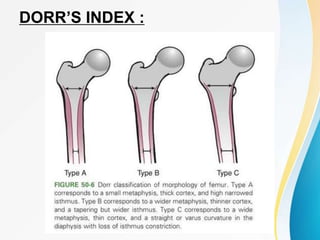
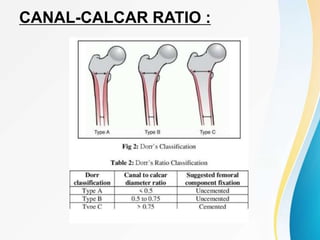
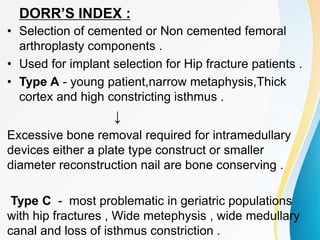
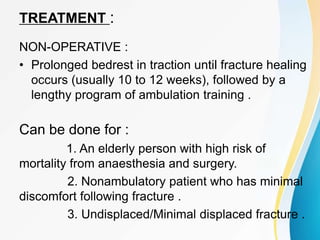
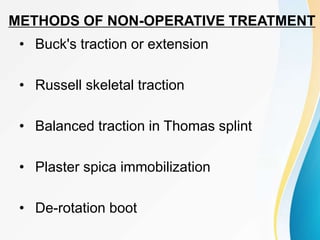
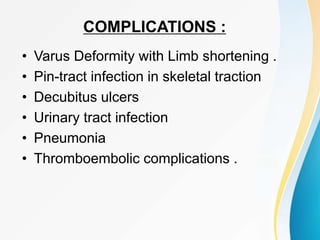
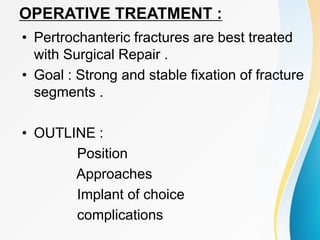
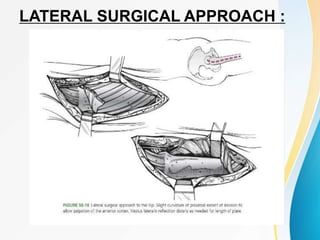
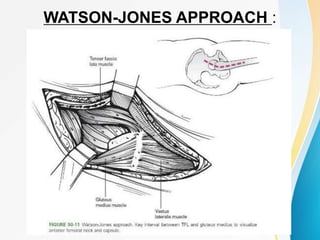
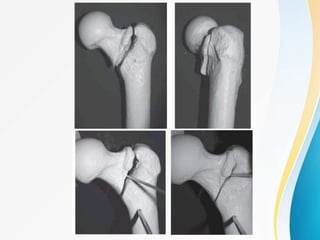
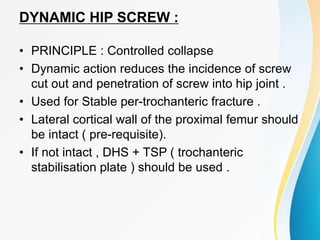
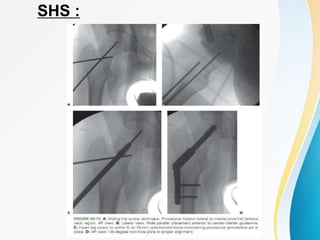
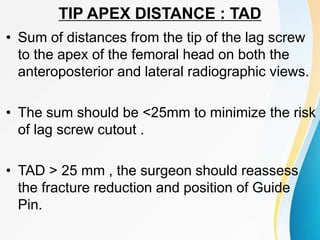
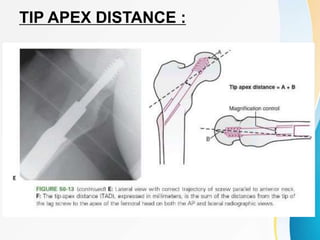
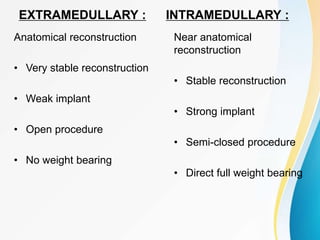
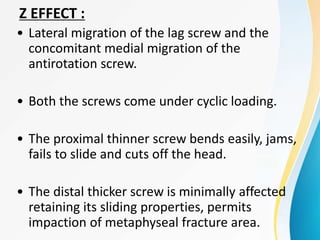
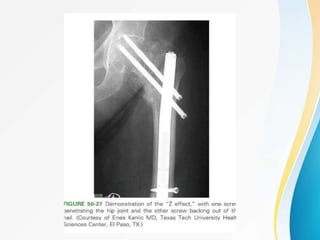
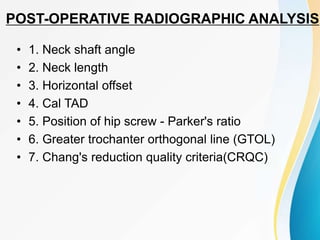
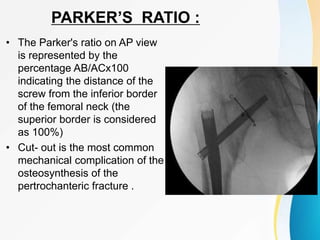
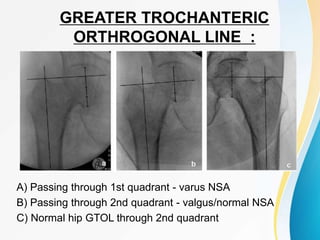
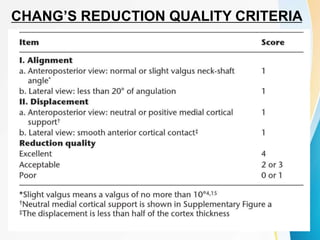
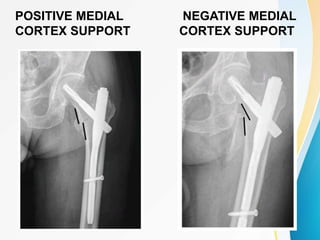
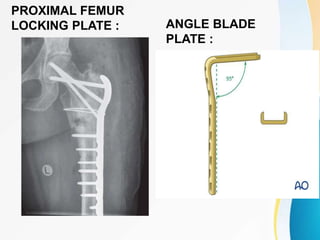
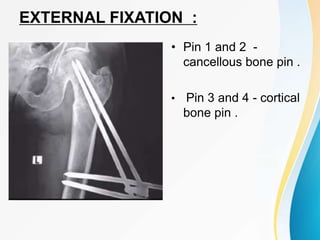
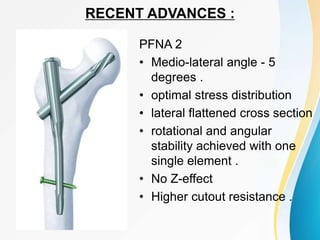
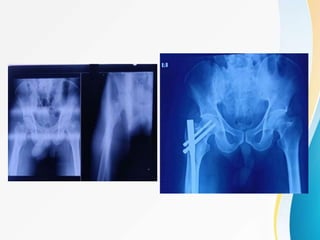
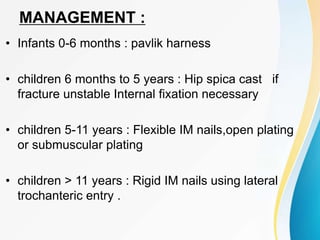
Trochanteric fractures occur in the region between the greater and lesser trochanters of the femur. They were traditionally treated conservatively but surgical fixation using devices like the sliding hip screw and proximal femoral nail are now preferred. Key factors in operative treatment include implant choice, surgical approach, and postoperative analysis of fixation parameters like tip-apex distance to minimize complications like screw cutout.