This document provides information on proximal humerus fractures, including:
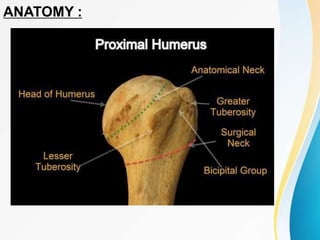
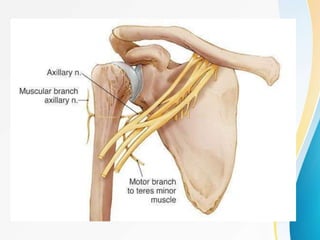
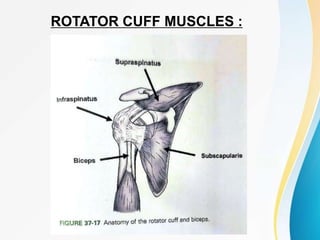
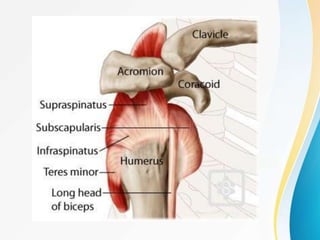
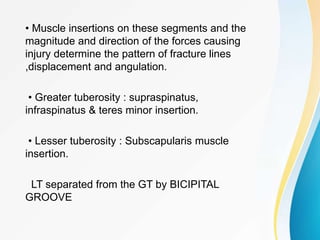
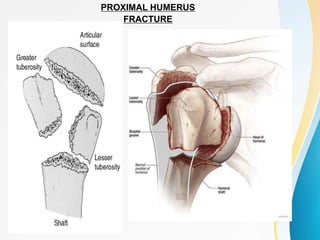
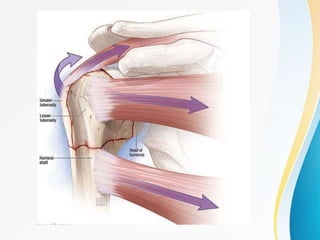
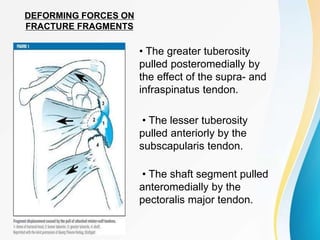
1. The anatomy of the proximal humerus and forces that cause deformity.
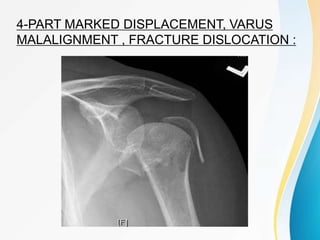
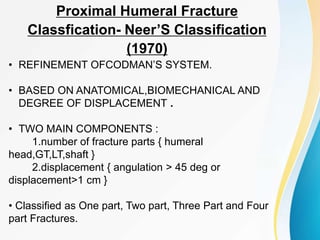
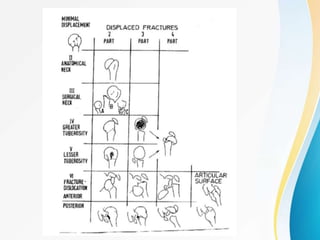
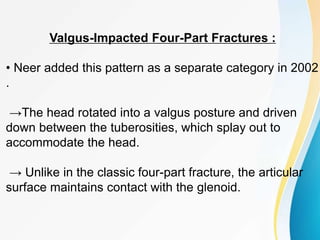
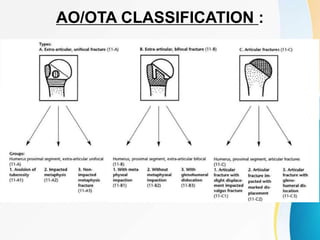
2. Classification systems for proximal humerus fractures including Neer's classification.
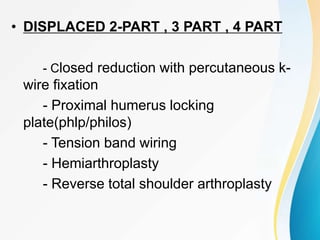
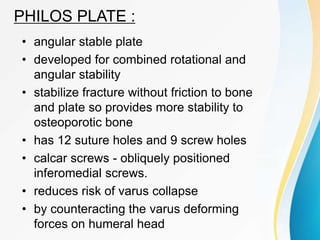
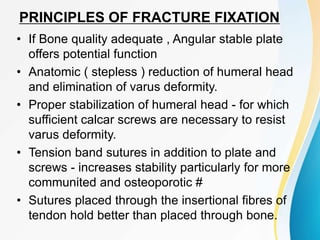
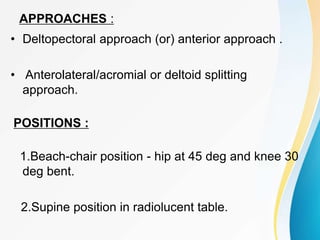
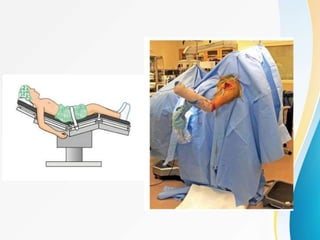
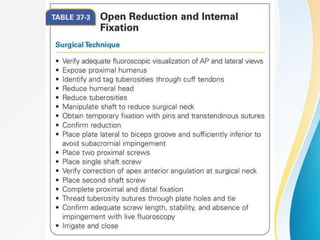
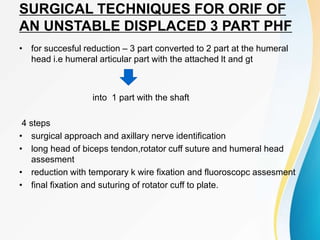
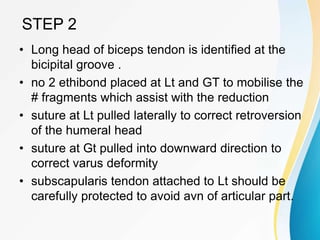
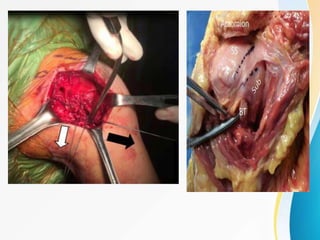
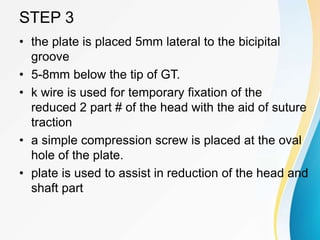
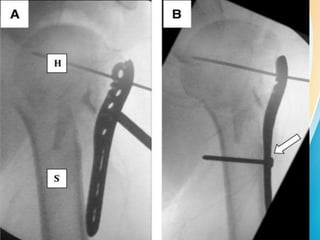
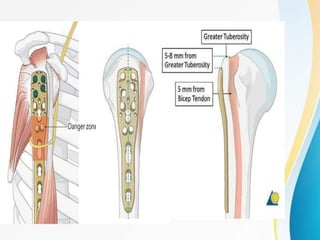
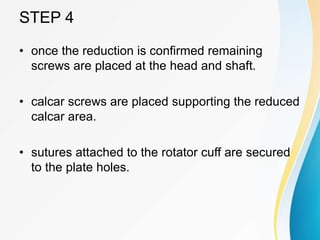
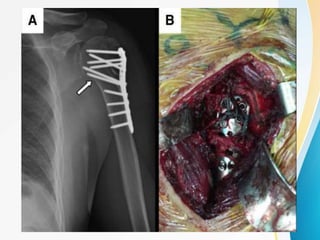
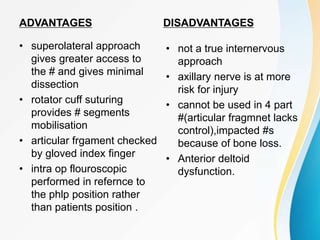
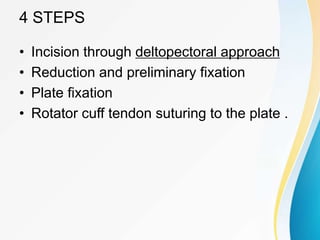
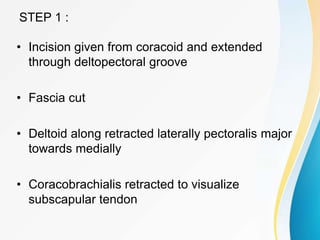
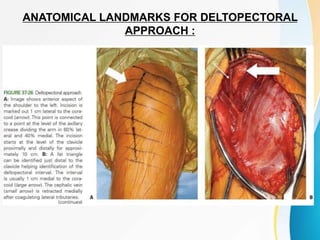
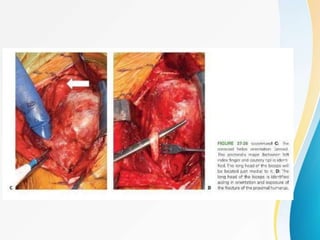
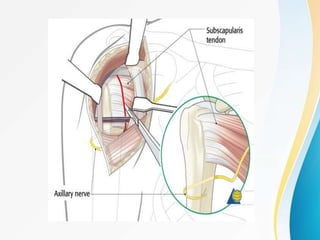
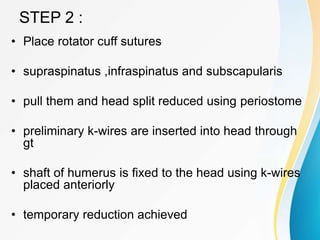
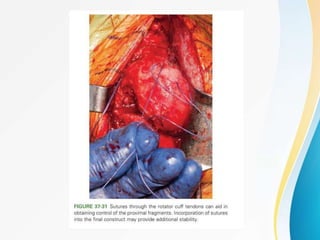
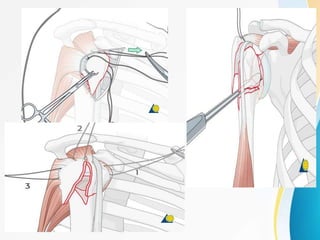
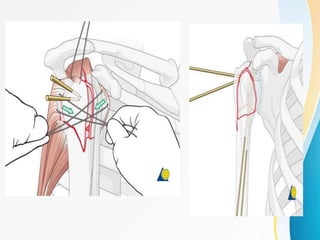
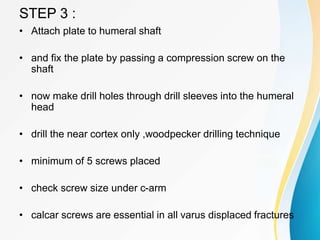
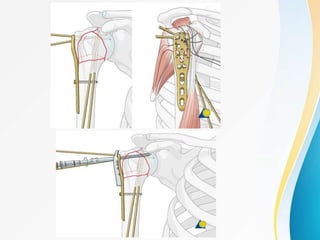
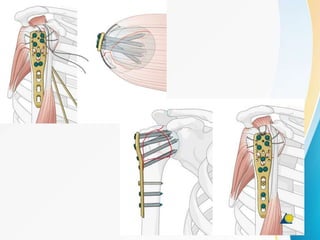
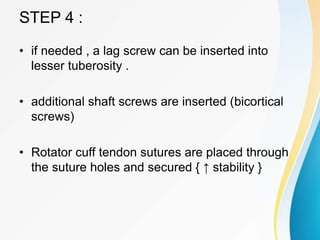
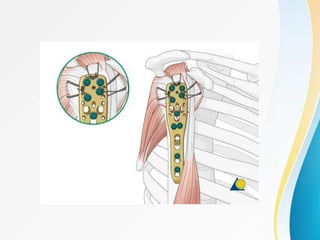
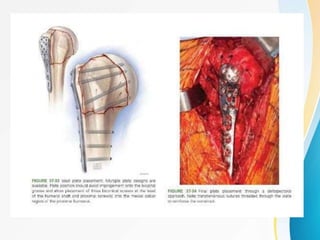
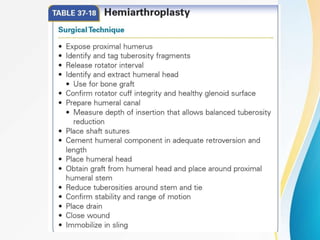
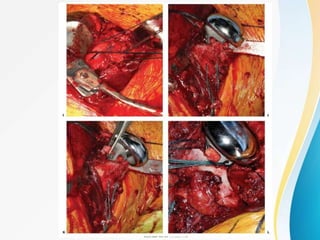
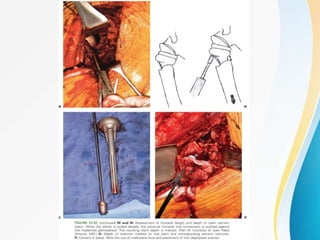
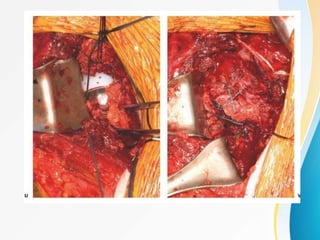
3. Surgical techniques for open reduction and internal fixation of displaced proximal humerus fractures using a proximal humerus locking plate. The procedure is described in 4 steps.
![Mechanism :
• Old Pts low energy trauma. [FOOSH]
• Young Pts – High energy trauma
• Most # are nondisplaced, good prognosis –
nonsurgical
• Risk factors: osteoporotic bone ,impaired
vision & balance, medical comorbidities,
decreased muscle tone and Seizures &
electric shock (indirect causes)
• Severe soft tissue disruption always
require surgical intervention](https://image.slidesharecdn.com/1proximalhumerusfracturessurgicalmanagementphilosplatingfinal-230722102714-d1a6329d/85/1PROXIMAL_HUMERUS_FRACTURES_SURGICAL_MANAGEMENT_PHILOS_PLATING_FINAL-pptx-14-320.jpg)







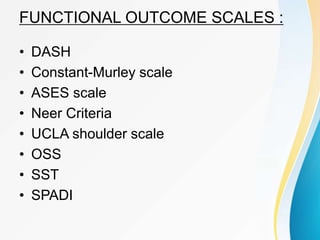
![DASH
• Disabilities of the Arm, shoulder, and Hand
scale [ DASH ]
• Most widely used shoulder scale for
outcome assessment .
• Pt based , 6 domains {Daily activity ,
symptoms ,social Fn,Work Fn ,sleep,
confidence}.
• 30 questions and each question rated on a
likert scale 1 to 5 .
• Quick DASH - 11 questions](https://image.slidesharecdn.com/1proximalhumerusfracturessurgicalmanagementphilosplatingfinal-230722102714-d1a6329d/85/1PROXIMAL_HUMERUS_FRACTURES_SURGICAL_MANAGEMENT_PHILOS_PLATING_FINAL-pptx-43-320.jpg)