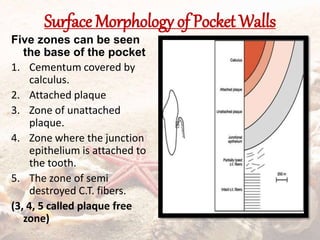
The document defines and classifies periodontal pockets. Key points:
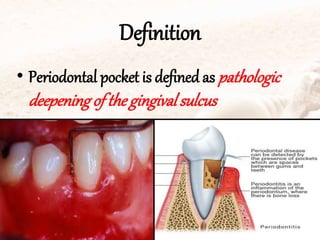
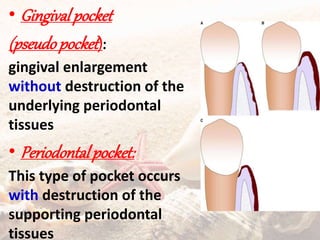
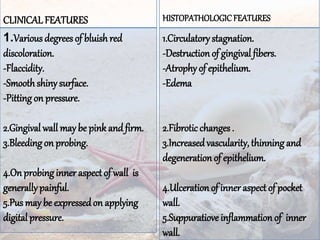
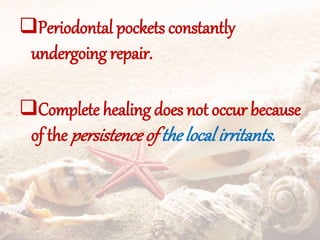
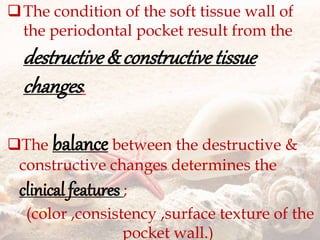
- Periodontal pockets are pathologically deepened gingival sulci with destruction of supporting tissues.
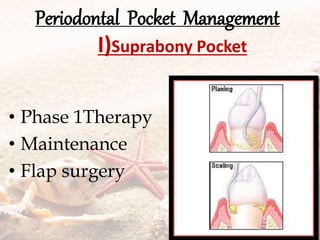
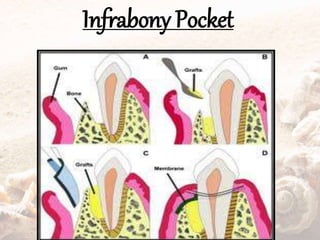
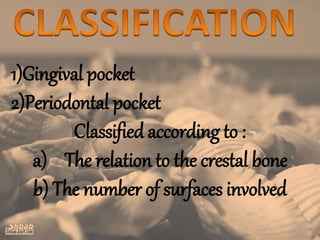
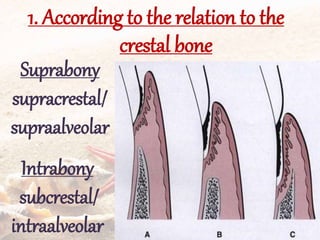
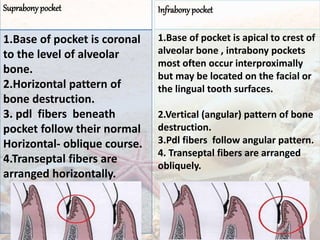
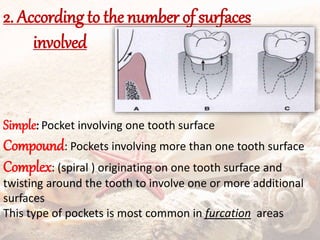
- They are classified as suprabony, infrabony, or furcation pockets based on their location relative to alveolar bone.
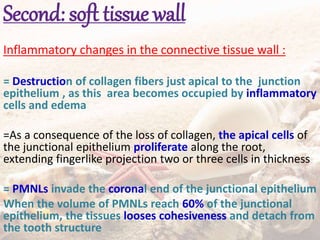
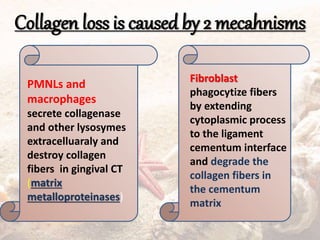
- Periodontal pockets contain plaque, microorganisms, inflammatory cells and products that drive the pathogenesis of periodontitis through host immune response and tissue destruction.
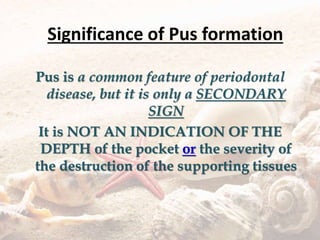
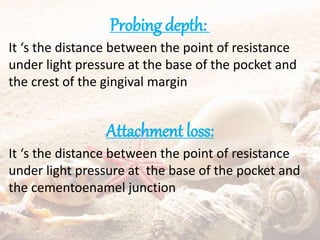
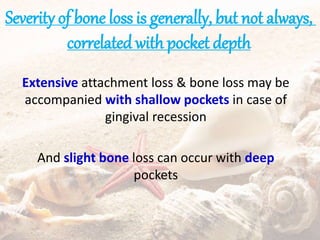
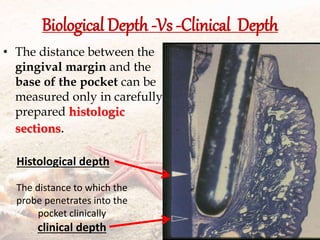
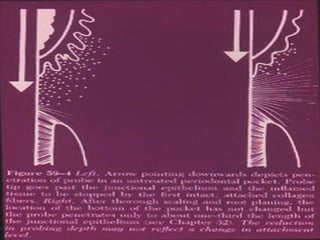
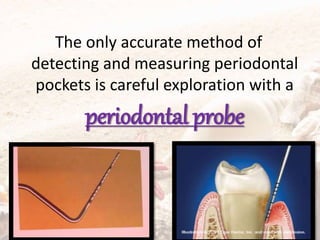
- Probing depth measures pocket depth while attachment loss measures loss of supporting tissues from their original position. Pocket depth does not always correlate with severity of bone loss.



![Simvastatin (SMV) is a specific competitive inhibitor
of 3-hydroxy-2-methyl-glutaryl coenzyme-A
reductase.
Pardeep et al [35] showed :
a greater decrease in gingival index and probing
depth and a clinical attachment level gain at sites
treated with scaling and root planing plus locally
delivered SMV gel in patients with chronic
periodontitis.
PradeepAR, Thorat MS. Clinical effectof subgingivally deliveredsimvastatinin the
treatment of patients withchronicperiodontitis: a randomizedclinical trial. JPeriodontol.
2010](https://image.slidesharecdn.com/periodontalpocket-150319001826-conversion-gate01/85/Periodontal-pocket-60-320.jpg)