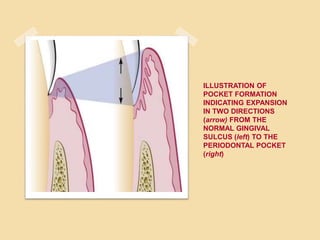
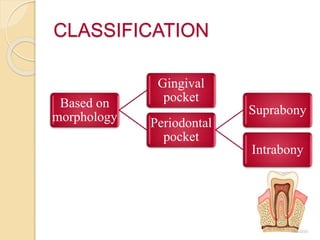
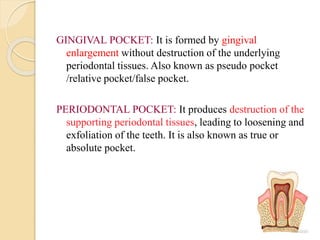
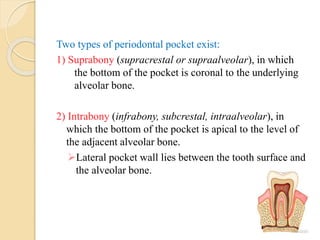
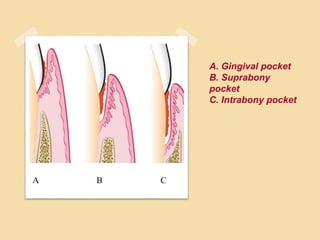
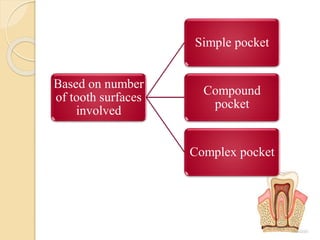
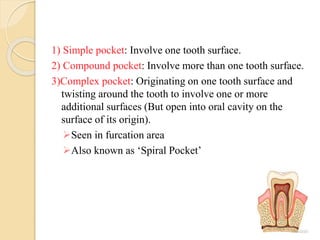
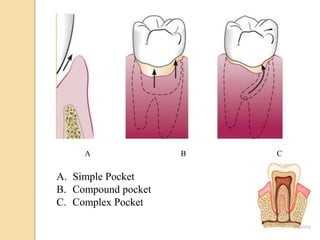
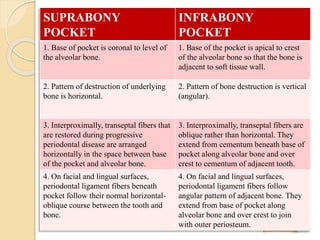
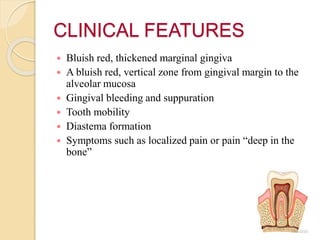
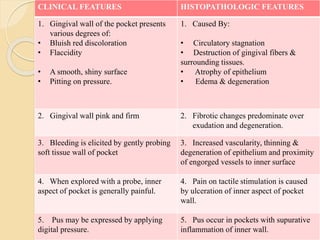
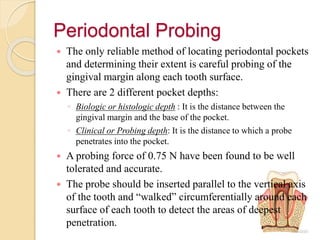
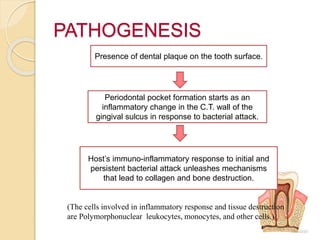
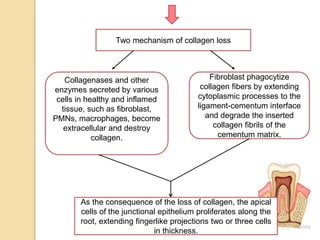
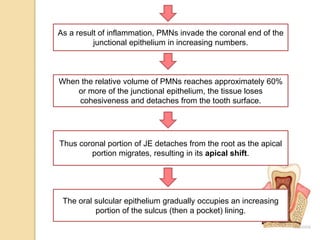
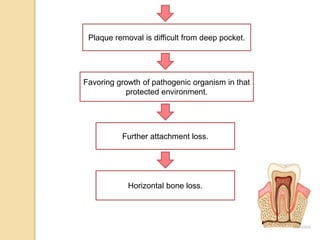
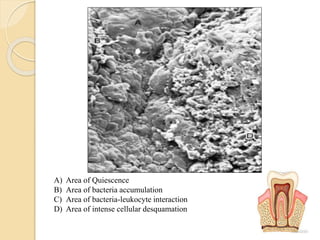
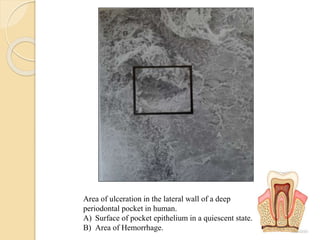
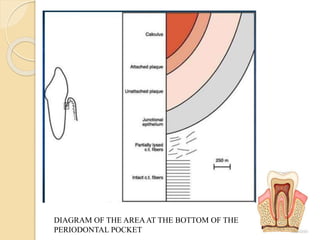
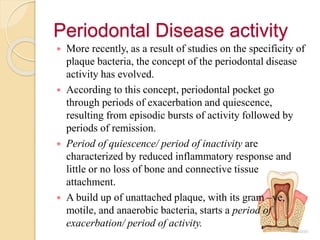
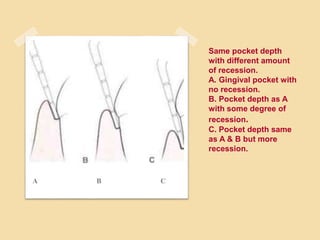
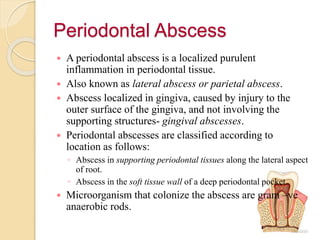
This document discusses periodontal pockets, including their classification, clinical features, pathogenesis, and histopathology. Periodontal pockets are pathologically deepened gingival sulci that can form through coronal movement of the gingival margin, apical displacement of the gingival attachment, or a combination. They are classified based on their morphology (gingival vs periodontal) and number of tooth surfaces involved (simple, compound, complex). Periodontal pockets develop due to bacterial plaque initiating an inflammatory response and host tissue destruction through the action of leukocytes and enzymes. Histologically, the soft tissue wall shows inflammation and the junctional epithelium is shortened.