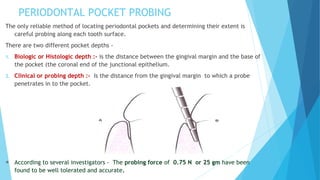
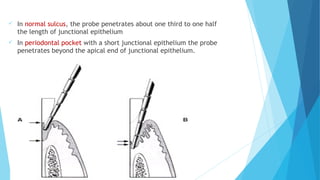
The periodontal pocket is a pathologically deepened gingival sulcus that is a key sign of periodontal disease. Pockets can be classified based on their morphology, relationship to crestal bone, number of tooth surfaces involved, soft tissue walls, and disease activity. The pathogenesis involves bacterial plaque that leads to inflammation, collagen loss, and detachment of the junctional epithelium from the tooth, forming a pocket. Pockets contain debris and can promote further attachment and bone loss if left untreated. Treatment involves non-surgical approaches like scaling and root planing or surgical procedures to reduce pocket depth.