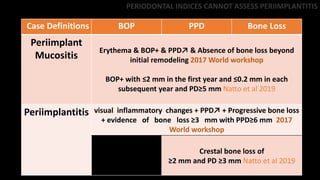
The document discusses key concepts regarding peri-implantitis and peri-implant mucositis. Some of the main points made include:
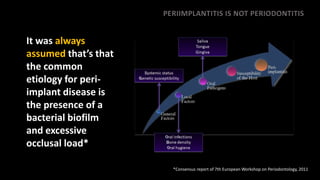
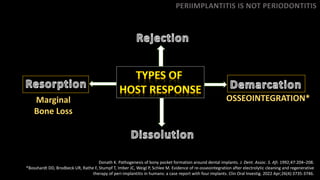
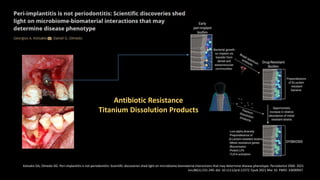
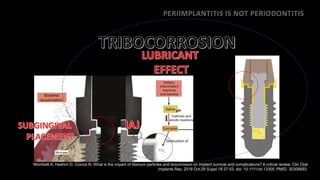
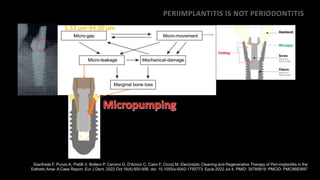
1) Peri-implantitis is not the same as periodontitis and should be considered a distinct disease process with its own diagnostic criteria and treatment approaches.
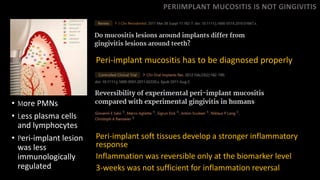
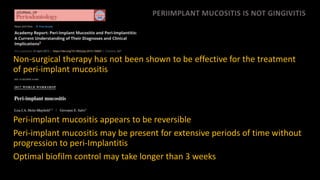
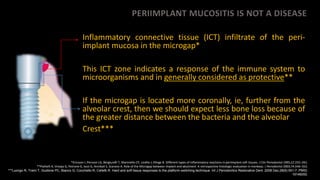
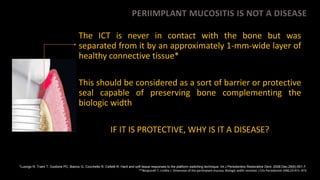
2) Peri-implant mucositis is also distinct from gingivitis and may require longer than 3 weeks for resolution of inflammation.
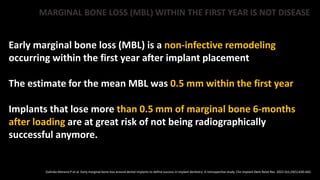
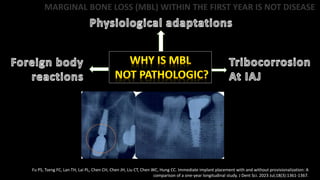
3) Some amount of marginal bone loss within the first year of implant placement should be considered normal remodeling rather than a disease process.
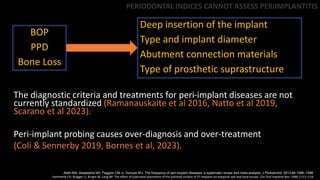
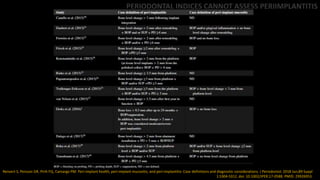
4) Periodontal indices alone cannot adequately assess peri-implant health and disease status due to differences in