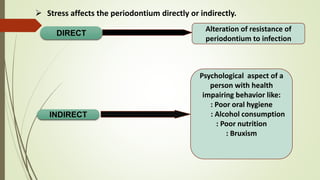
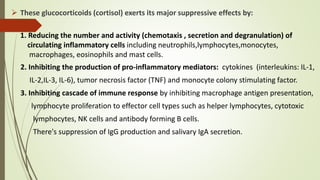
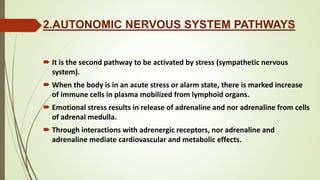
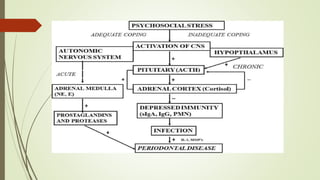
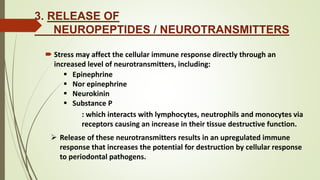
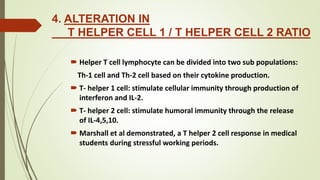
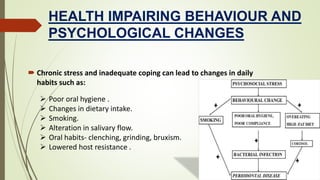
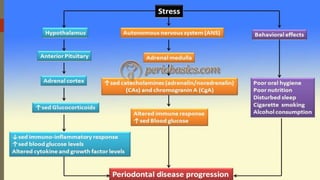
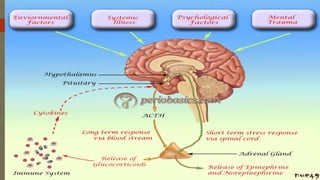
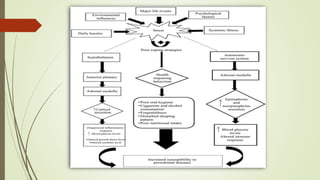
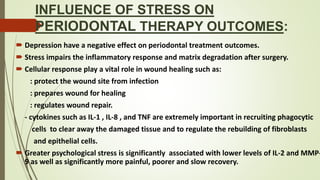
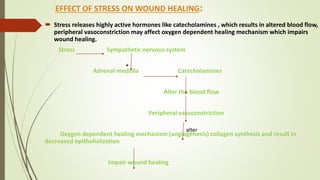
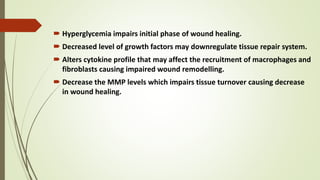
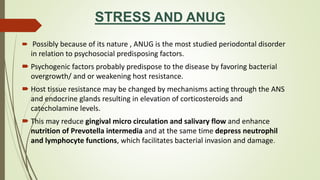
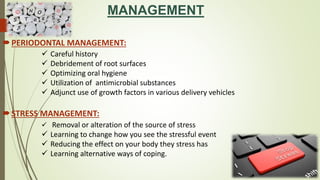
Stress can negatively impact periodontal health through both direct and indirect means. Prolonged stress can cause immunosuppression by increasing cortisol and altering the immune response. It can also lead to unhealthy behaviors like poor oral hygiene, smoking, and bruxism. Stress has been linked to periodontal diseases like ANUG and aggressive periodontitis. It can impair wound healing after periodontal treatments and influence treatment outcomes. Managing stress may benefit periodontal disease treatment and prevention.