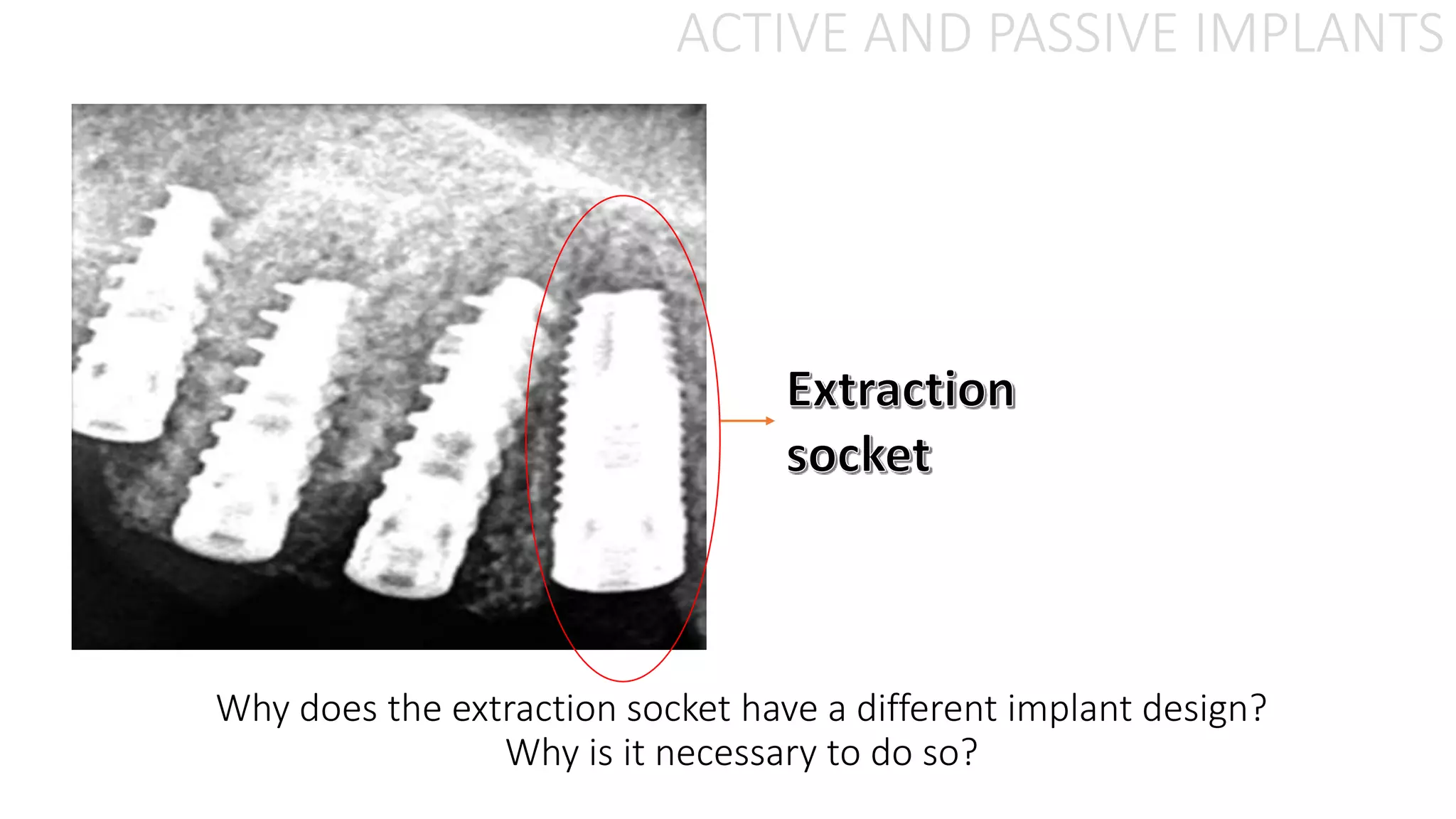
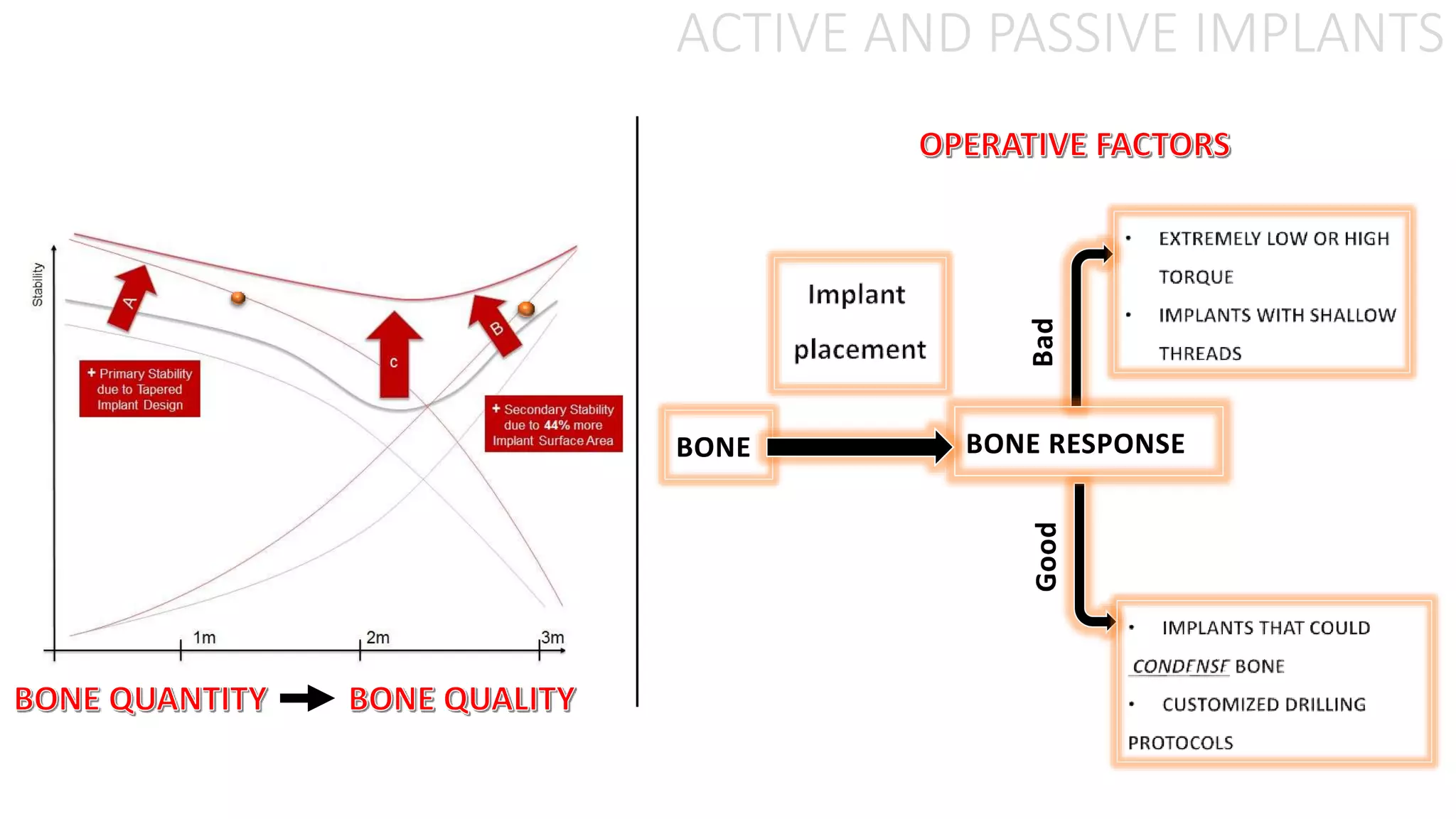
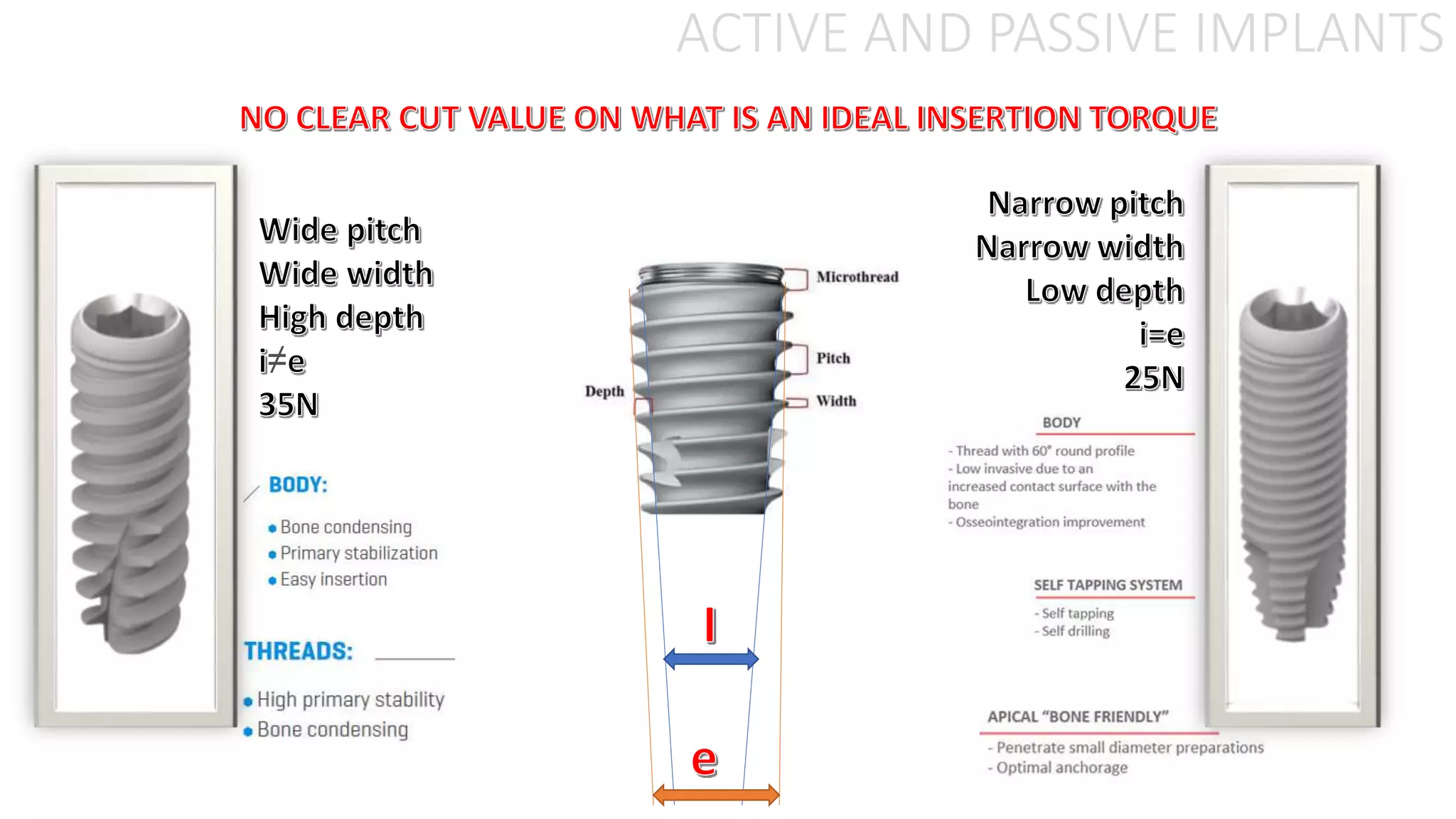
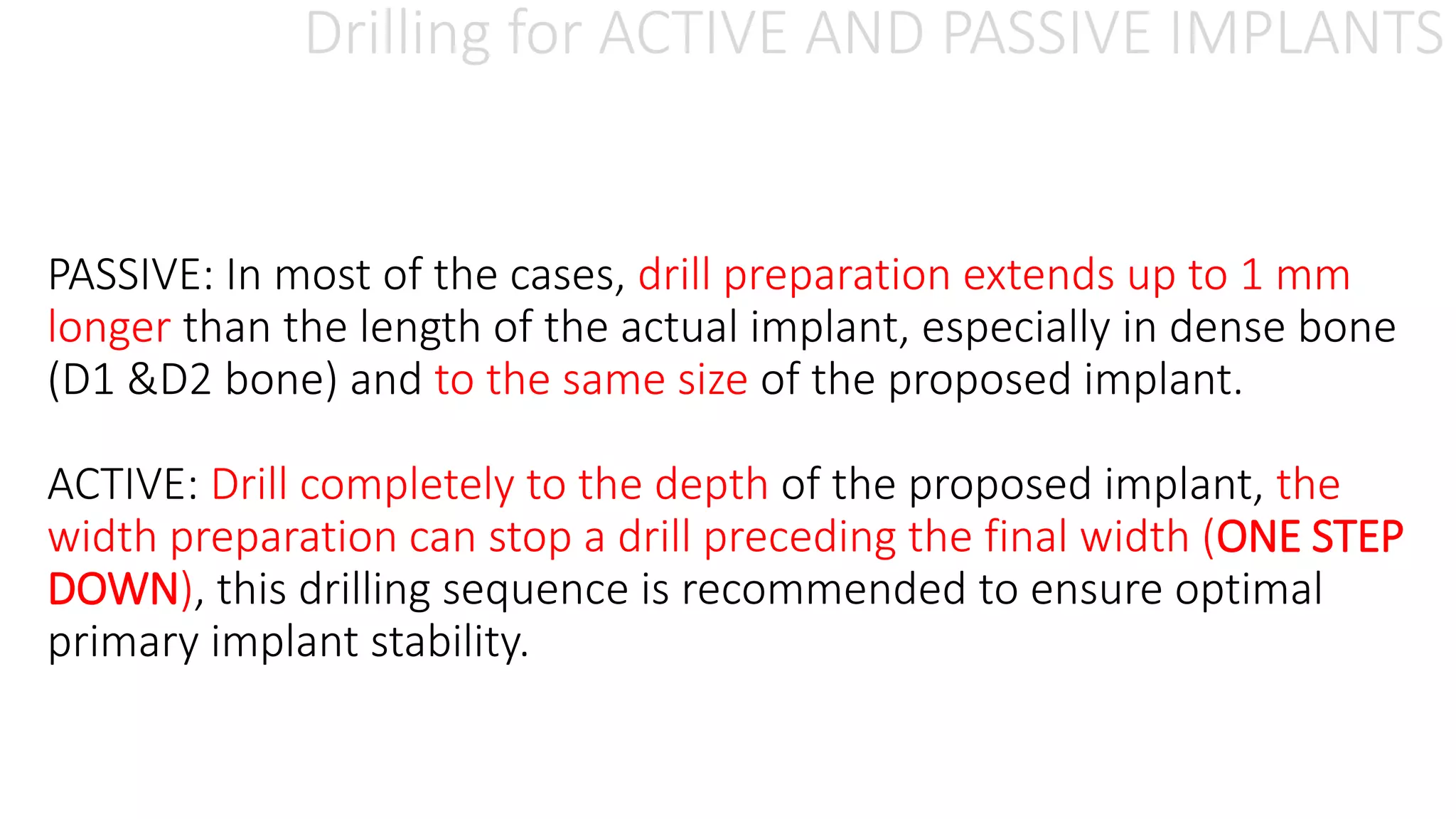
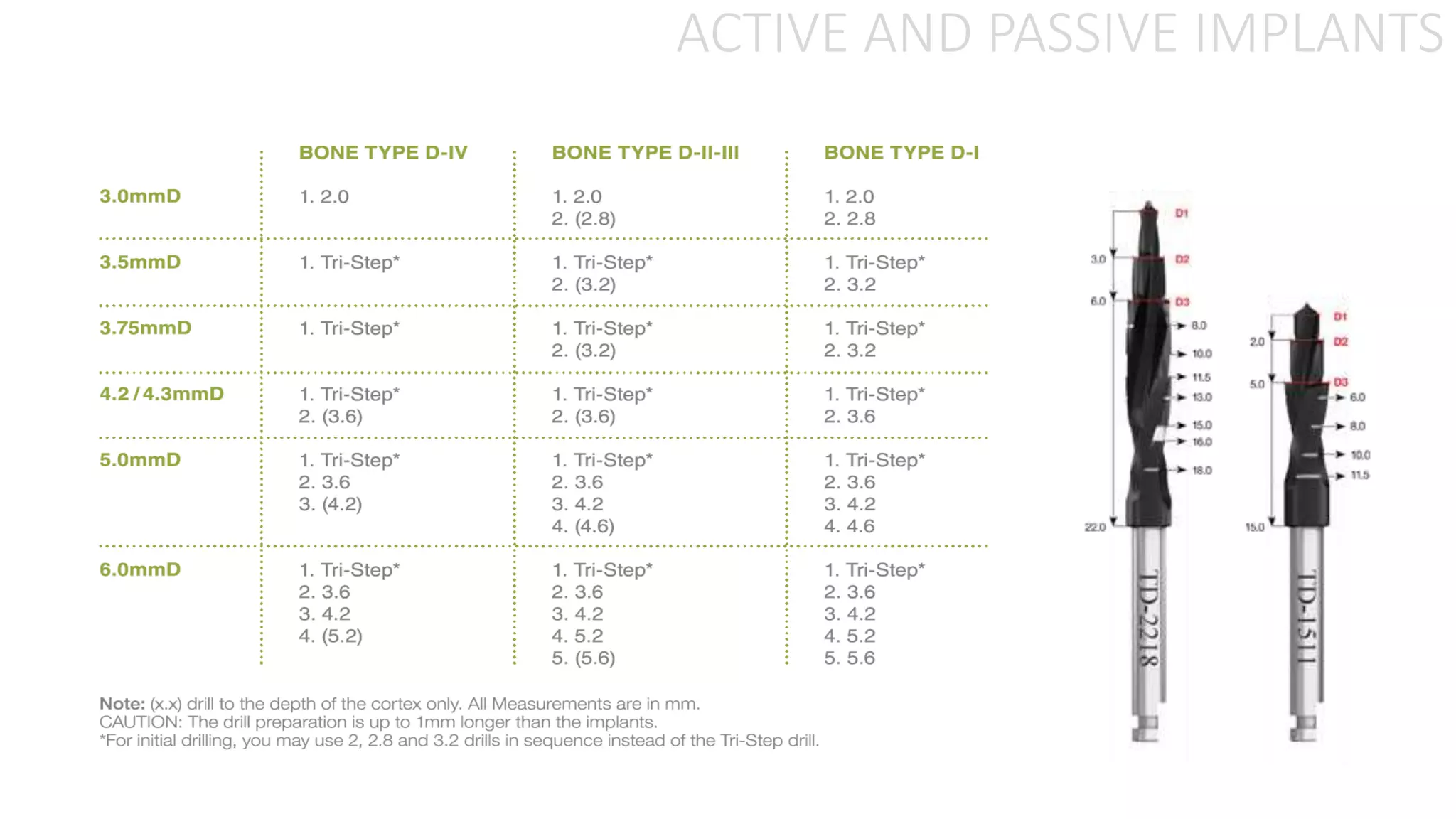
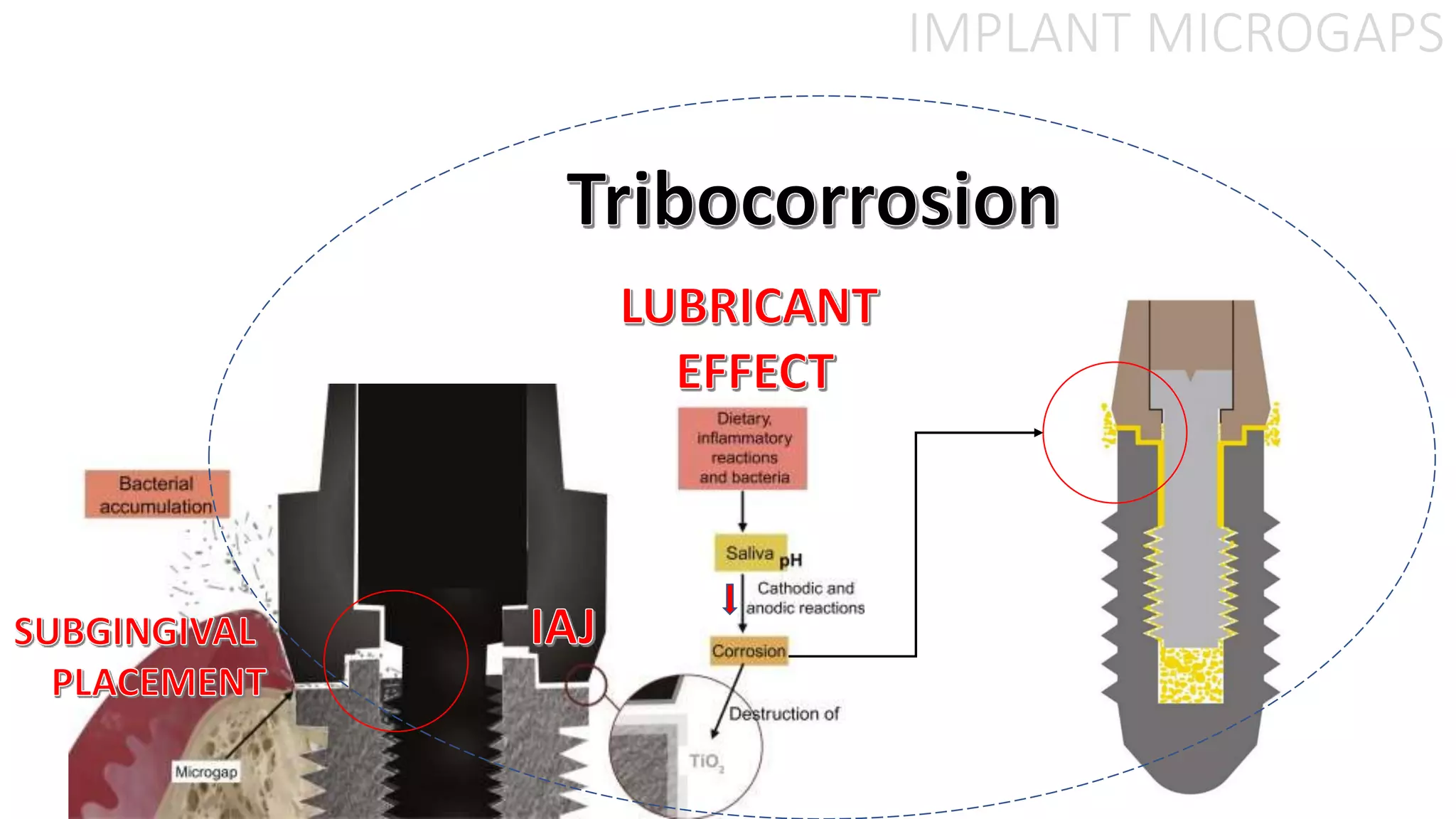
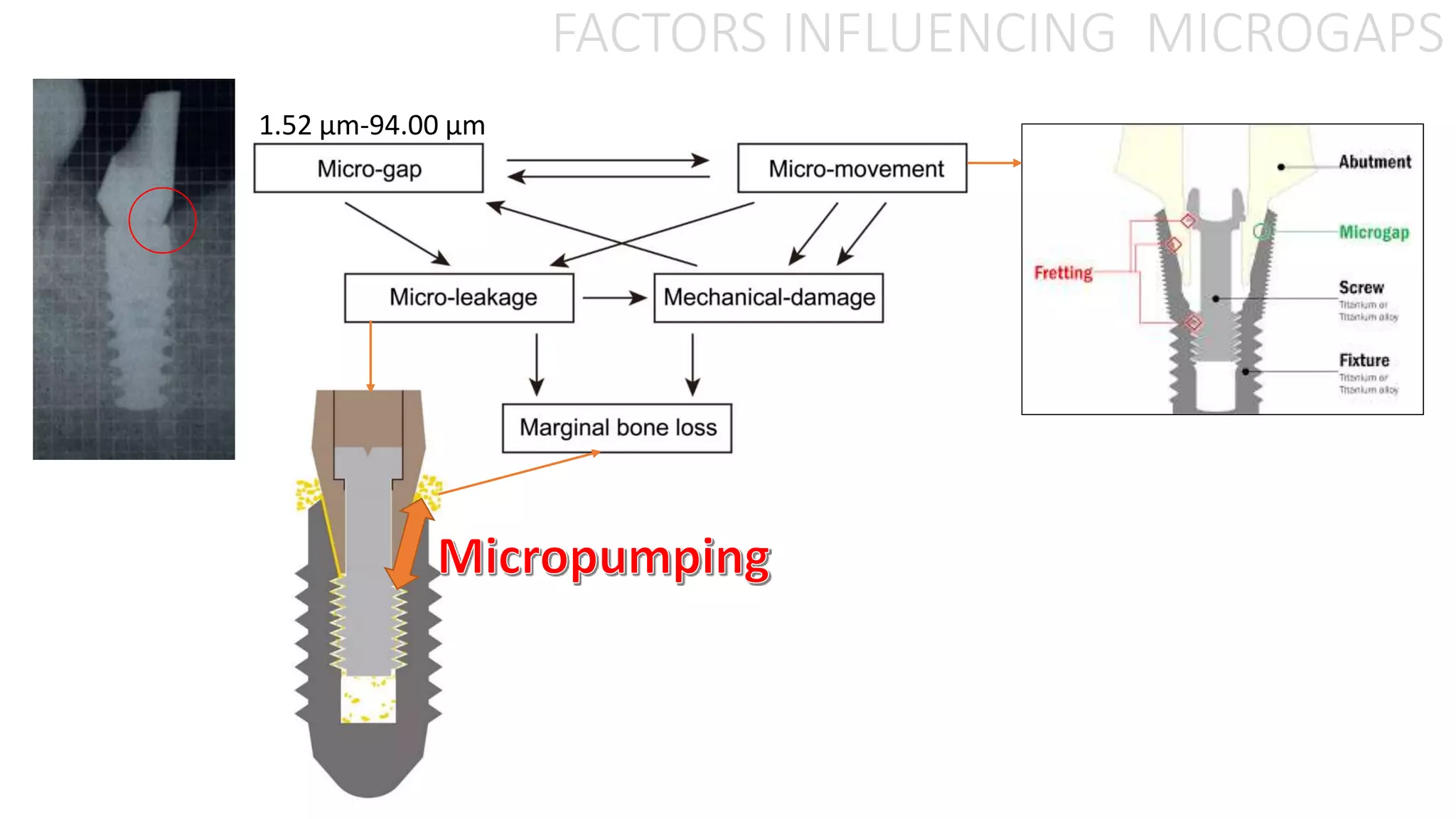
The document discusses the differences between active and passive implants, how they are placed, and factors that influence microgaps between the implant and bone. For passive implants, drilling extends 1mm beyond the implant length to allow for density differences in bone quality. Active implants are drilled to the exact depth and slightly less than the full width to ensure optimal stability. Microgaps between implants and bone can range from 1.52 to 94 micrometers and influence the bone response.