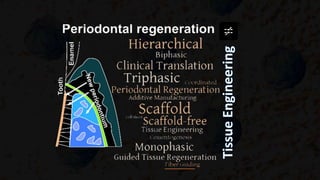
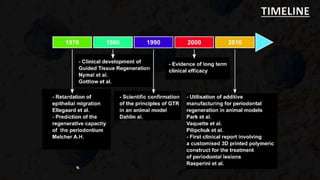
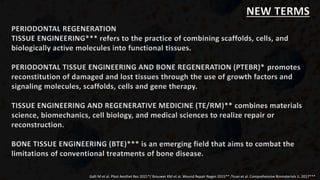
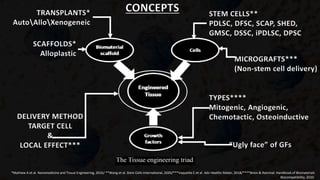
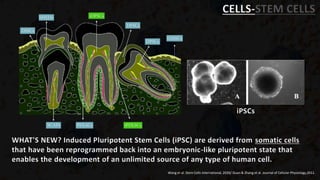
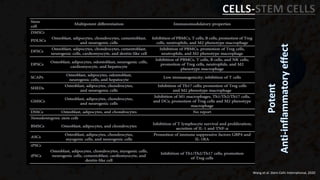
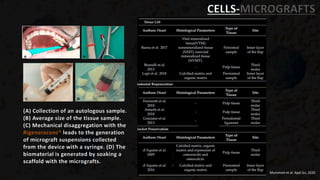
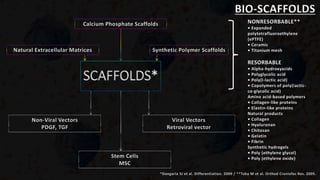
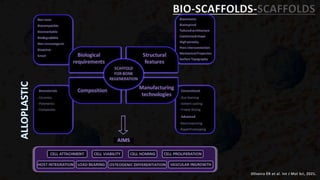
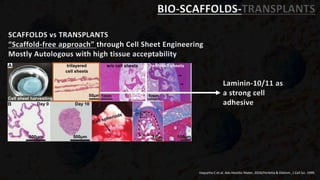
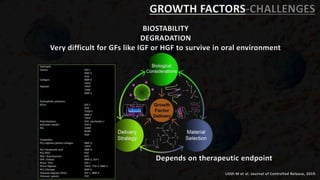
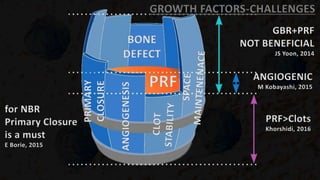
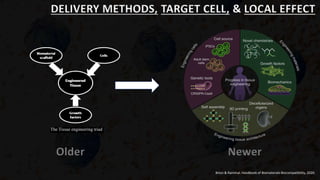
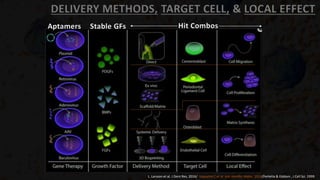
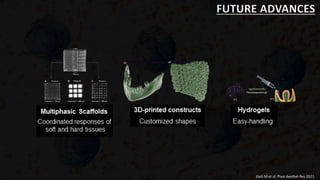
Tissue engineering aims to combine scaffolds, cells, and growth factors to regenerate tissues. Periodontal tissue engineering specifically focuses on regenerating damaged periodontal tissues through the use of scaffolds, stem cells, growth factors, and gene therapy. Tissue engineering combines materials science, cell biology, and medical sciences to repair or reconstruct tissues. Bone tissue engineering is an emerging field that uses these techniques to treat bone diseases by overcoming limitations of traditional treatments.